Initial rg signs of osteochondrosis. Signs of osteochondrosis in the cervical, thoracic and lumbar spine in men or women. Causes of pain
Lumbar osteochondrosis is one of the most common forms of the underlying disease, osteochondrosis itself. Lumbar osteochondrosis, the symptoms of which are equally defined in both men and women, manifests itself in the form of pain concentrated within the region of the sacrum, reflected in its symptoms and on the lower extremities, which is often self-defined by patients as "pinched lumbar nerve".
general description
Most often, the considered form of osteochondrosis develops against the backdrop of back injuries and a sedentary lifestyle, respectively, automatically at risk for the possibility of developing this disease are people whose professional activities include loads that affect the back. And these are not only office workers, who certainly belong to this group, but also porters, builders, service workers (waiters, for example), drivers, etc.
An important role is also given to the factor of heredity in the context of consideration of thoracic osteochondrosis. Here, not a lot, not a little, but about 60% of the probability is present in the presence of the disease in the next of kin. The rest of the body is affected by environmental factors that in one way or another affect the spine.
Lumbar osteochondrosis, like its other forms, is characterized by pain sensations of varying severity, which can be aching, occurring after sleep or when staying in the same position for a long time (with prolonged sitting, standing), as well as shooting and sharp. In the latter version, they arise as a result of a long-term adoption of a position that is not very comfortable, while at the same time it is impossible in such a situation to implement actions aimed at unbending, thereby excluding such a position along with the load provided by it. Actually, pain sensations arise as a result of pinching with the appropriate action of the nerve roots, as well as irritation of the nerves in the spinal column, irritation of the ligaments and muscles (focused within the area of innervation, that is, the actual location of the nerves of the department of the area under consideration that controls it) and edema.
It is important to note that in an isolated form this type of osteochondrosis is extremely rare, and therefore most often the course of the disease is combined with the symptoms inherent in cervical osteochondrosis, we will consider it in our next article.
The common and earliest symptom that is relevant for all forms of osteochondrosis, as we have already noted, is the manifestation of pain, which in this case is determined by a specific localization, that is, back pain. The spread (irradiation) of pain can be noted to the thighs and buttocks, as well as to the legs (from their outer surface).
The term used to define osteochondrosis in its more detailed version (degenerative-dystrophic lesion), which is relevant for the intervertebral disc, actually implies a complex of pathological conditions that are significant in its diversity, directly related to various types of structures of the spine (vertebral column), and with disks, joints and osteophytes. The same problems that are directly related to the defeat of the disc are its protrusion and discogenic pain.
Protrusions in lumbar osteochondrosis
Protrusions in this area of interest to us develop most often, moreover, it is protrusions that cause pain in the lower back. The lumbar region itself, given its location and features, is most prone to the occurrence of certain functional problems.
That is, when considering this statement on the one hand, it can be distinguished that our center of gravity directly relates specifically to the lumbar region, respectively, it is on it that a significant part of the loads falls. When viewed from the other side, one can notice that a significant amplitude of movements, again, falls precisely on this, the lumbar region. Given this, the greatest tendency to damage (as well as protrusions of interest to us) falls on the discs concentrated in the lumbar region. In addition, we must not forget that changes in the discs in this and, of course, in other areas, occur, including against the background of age-related degenerative processes.
Let us remind our readers what protrusions actually are. The connection of the discs to each other in the spine is provided by discs based on cartilage tissue. The main components of the intervertebral disc are the nucleus pulposus and the annulus fibrosus, through which fixation is provided within the framework of the vertebral disc. The impact of certain factors and conditions provokes the possibility of rupture of this ring, against which, in turn, the nucleus protrudes outward. As a result of this process, a hernia develops. As for protrusion, it is already developing as a result of a similar course of the process, but without a concomitant rupture of the ring - in this case, it is simply subject to thinning, and not rupture, because the core protrudes right through the ring. Actually, this protrusion is defined as a protrusion.
As for the symptoms of protrusion, it manifests itself in the following:
- feeling of stiffness in the lower back;
- pain in the lumbar region;
- pain in the lower back of a chronic nature;
- lumbosacral sciatica;
- numbness, pain, tingling of the toes, in the feet;
- violations of the functions of urination (in rare cases, the pathology under consideration).
It is mainly applied to the protrusion of the lumbar disc conservative treatment. Meanwhile, significant in the development of protrusions are often accompanied by severe symptoms that are resistant to treatment, in this case, you can not do without surgical intervention.

Lumbar osteochondrosis: symptoms
Pain in this form of osteochondrosis manifests itself in various intensity options. So, it can be aching pains, which appear mainly after sleep or after a long sitting, or there may be pains that shoot and are sharp in their manifestation. At the same time, the manifestation of the latter is often noted at the time of occupying an uncomfortable posture without the possibility of straightening. Any variant of pain is directly related to the effect on the nerve endings, to the swelling of the muscles, their irritation and to the pinching that the nerve roots are exposed to. Also, pain is associated with irritation of the ligaments of the lumbar region in the region of innervation of its nerve endings.
Increased pain in the lower back with the considered form of osteochondrosis is noted when coughing and sneezing, including movements made by the body (especially when bending forward).
Lumbar osteochondrosis can also manifest itself, in addition to back pain, also in the form of sensitivity disorders noted in certain areas (skin, lower half of the body, leg muscles). The weakening of the tendon reflexes in the legs or their complete disappearance is also not ruled out. As a rule, it is osteochondrosis that provokes the development of curvature in the lumbar spine.
Based on the specific plane of the actual curvature, osteochondrosis is divided into the following types:
- kyphosis - in this case, the smoothness of the lumbar region is noted, and often its arching back;
- lordosis - arching of the spine occurs forward;
- scoliosis - the spine curves to the left or right.
Pinching of the roots belonging to the spinal cord as a result of the development of osteochondrosis within the lumbar region is often defined as a number of specific disorders, namely defecation or urination disorders, disorders associated with sensitivity in the genital area or perineum.
As a rule, pains appear (and also become aggravated) as a result of the impact produced during physical exertion. Painful response in this case can be observed after this load, and after some time from the moment of its impact. Basically, patients' complaints in this regard are reduced to the appearance of dull and aching pain in the lumbar region, and in some cases it radiates to the leg, which is defined as lumbodynia. In addition, there may be complaints about the appearance of pain in the leg with its intensification at the time of trying to lift something heavy (). The same applies to sneezing and coughing, shaking driving, changing the position of the body, as well as staying in the same body position for a long time.
As a result of the exacerbation of the disease in question, there is a constant and pronounced tension on the part of the back muscles, which manifests itself in the impossibility of implementing actions aimed at straightening or moving. Any movement is accompanied by increased pain. In addition, even with a short stay of the patient in cold conditions, he has acute lumbar pain (which is also defined as "lumbago").
Symptoms of lumbar osteochondrosis are also manifested in the following:
- violation of sensitivity from the side of the thighs, buttocks, legs, in the foot (which is noted somewhat less frequently);
- spasm of the arteries of the feet, increased chilliness of the legs;
- tingling that occurs in the legs, "goosebumps";
- peeling of the skin and its dryness in the area in which there is usually a loss of sensitivity or pain;
- sweating disorders.
As the most inherently unpleasant complication that occurs against the background of osteochondrosis, one can single out the instability of the vertebrae, in which the disc ceases to properly fix the vertebra. This, in turn, provokes a “slipping” under the influence of gravity of the lumbar region from the sacrum when the load is exerted on the lumbar region. As a result of this, not just unpleasant violations can develop, but dangerous violations that already affect the work of internal organs. In particular, the genitourinary system “suffers”, this manifests itself in men in the form of problems with potency, and in women in the form of problems relating to the appendages, uterus and ovaries.
Manifestations of lumbar osteochondrosis
In accordance with the most complete classification, there are a number of specific syndromes that are relevant for lumbar osteochondrosis. In particular, these include the following syndromes:
- reflex syndromes - these include lumboishalgia, lumbalgia and lumbago;
- radicular syndromes - vertebrogenic (or discogenic) sacro-lumbar sciatica, the course of which is accompanied mainly by damage to the first sacral root or fifth lumbar root;
- radicular-vascular syndromes - radiculo-ischemia, which manifests itself in the form of a process of squeezing blood vessels (in particular, veins or arteries are subject to compression), while squeezing is performed simultaneously with the root.
Let us briefly highlight what the listed syndromes are.
Lumbalgia in particular, refers to a chronic type of pain that occurs gradually after long-term adoption of an uncomfortable body position or after prolonged sitting, as well as after the impact on the body and a specific area after exercise.
Lumbago manifests itself in the form of acute lumbar pain, characterized as a "backache", mainly lumbago occurs at the time of lifting weights or when the movement is unsuccessful. Sometimes lumbago is also noted after coughing or sneezing.
Radicular syndromes (radiculitis) manifest themselves in the form of compression of the roots (one or two) in combination with the accompanying symptoms. In particular, this is radicular pain, disturbances of sensory and motor functions. In terms of sensory function, we are talking about a loss of functionality of the damaged root, and in terms of motor function, impairments are noted in the weakness of the flexors / extensors of the foot or thumb.
Concerning radiculoischemia , then it already appears against the background of compression noted in the area of concentration of the radicular-spinal arteries. In the clinic of manifestations, gross forms of motor disorders (in the form of paresis and paralysis), as well as sensory disorders that occur in one form or another, both with weak pain in their severity, and in their absence (which is also possible, although more rare cases).
Diseases associated with lumbar osteochondrosis
Lumbar osteochondrosis occurs not only in combination with pain and other listed symptoms, but also in combination with some characteristic diseases of the internal organs.
Thus, about 30% of patients with a clinic relevant for lumbar osteochondrosis note the presence of certain problems associated with the liver or with the functions of the gastrointestinal tract. The fact is that the presence of one or another disease of the gastrointestinal tract, pancreas or liver provokes, along with pain impulses, vascular and muscle tension and spasm, resulting in a condition oxygen starvation with simultaneous development in certain areas of the body of the dystrophic process. The aggravation of the process occurs with a metabolic disorder, which is inherent in this type of disease.
In addition, as we have already noted earlier, lower back pain can provoke the development of diseases in the pelvic organs. Women may experience such a disease as inflammation of the appendages (which is defined as), and men, in turn, experience all the "charms", that is, inflammation of the prostate gland.
The manifestations of lumbar osteochondrosis are also accompanied by congestive phenomena in the pelvic area, which develop as a result of the above diseases, including both with and with.
Treatment
Mostly, the treatment of osteochondrosis is multicomponent and rather complicated in its implementation. Mostly all measures of therapy are reduced to the following points:
- drug treatment;
- if necessary, surgical treatment;
- diet;
- physiotherapy.
Exacerbation of the disease requires, first of all, patient bed rest. The main recommendation for this part is a hard/hard sleeper. Seizures that are extremely pronounced in manifestations require a minimum motor load and an early referral to the appropriate specialist.
Osteochondrosis in medicine is called dystrophic changes in the intervertebral discs. Such a problem can appear in a person absolutely at any age. Impairment of function can provoke the development of many unpleasant concomitant health problems. Therefore, it is necessary to immediately pay attention to the signs of osteochondrosis of the cervical region, and then proceed to immediate treatment.
General description of the disease
The cervical spine includes 8 paired nerve nodes, and 7 usually develops due to the fact that the intervertebral pulp degenerates into vitrified tissue. In parallel with this, pathological changes also adversely affect the termination of nerve fibers, as well as important vessels. Basically, this pathology affects the 8th and 7th vertebrae.
Signs of cervical osteochondrosis are very easy to confuse with other pathologies. During the disease, headache attacks are observed, as well as discomfort in the neck. Signs of cervical osteochondrosis are also accompanied by dizziness, nausea, and pressure problems. In most cases, this disease is confused with diseases of the vessels and heart.
It is important to note that often, against the background of a pathology with vertebrae, the patient begins to lose consciousness abruptly, feels a lack of air, and sometimes even the tongue may become numb. Therefore, the signs of osteochondrosis of the cervical region must, as they say, "know in person."
This unpleasant disease is diagnosed mainly in people whose age is more than 30 years. This is due to the peculiarities of the location of the human skeleton, as well as constant dynamic and statistical loads. But it is worth paying attention to the fact that the disease has recently been rapidly getting younger, as a result of which signs of cervical osteochondrosis in women and men are observed even in adolescence.
Causes of the disease
The development of this unpleasant disease is influenced by pathological and physiological processes. All of them are closely related to each other, and in medical practice, specialists constantly consider them together.
As for physiological changes, they are caused by irreversible age-related processes that take place in the cartilage of the spine. These changes are localized in the central region of the intervertebral disc. Physiological signs of cervical osteochondrosis in women and men are manifested as pulp pinching by some fibrous tissues. When the nerve endings are irritated, the patient begins to experience discomfort.
Pathological changes are such a process when the area of inflammation goes beyond the zone of cartilage tissue. Pathological signs of osteochondrosis in women and men can cause severe irritation in the area of nerve endings, as well as pinching of blood vessels. Such changes can occur against the background of malnutrition, due to a sedentary lifestyle. In addition, pathological changes are often observed in adolescents and people belonging to the middle age category.
It is important to note that the signs of osteochondrosis of the cervical spine in women and men in some cases disappear on their own or appear as short-term episodes. The human body has many protective and compensatory functions, which for some time are able to level these pathological changes in the cartilage area.

Provoking factors
The following factors can provoke the development of this unpleasant disease:
- Excess weight.
- Lack of constant physical activity, as well as sedentary work.
- Stressful conditions and nervous loads.
- The patient's body is often in an uncomfortable position.
- Injuries in the back of the head and neck.
- Hypothermia.
It is also worth paying attention to the fact that signs of osteochondrosis of the cervical spine in men and women may appear due to a congenital anomaly, as well as due to autoimmune diseases.
Main features
It should be noted that cervical osteochondrosis is sometimes not accompanied by pain in a particular part of the spine. Quite often, this disease has a fuzzy clinical picture. The main signs of osteochondrosis of the cervical spine in men and women include dizziness, sudden changes in blood pressure, migraine. However, it is necessary to highlight the symptoms that require urgent hospitalization of the patient:
- Increasing headache, accompanied by a deterioration in general well-being.
- Loss of mobility of the muscles of the shoulder girdle or face, numbness.
- Violation of coordination of movements.
- Loss of consciousness.
Considering the signs and symptoms of cervical osteochondrosis, you should pay attention to the fact that pain is often given to the upper limbs and shoulder girdle. A distinctive feature in this case is the pain syndrome, which is paroxysmal in nature. Basically, such pain occurs after waking up, during laughter, sudden movements, sneezing and coughing.
Answering the question about what signs of osteochondrosis of the cervical region disturb the patient, one should pay attention to the fact that at the initial stage of this disease, the pain subsides quickly, a crunch in the neck is often observed, the muscles become weaker, and the skin loses its sensitivity.
If there are pathological changes in the sixth vertebra, then pain can be felt in the thumb. And if the changes affected the seventh vertebra, then the pain manifests itself on the middle finger.

Signs of osteochondrosis of the cervical and thoracic spine in women, as a rule, appear later than in the strong half of humanity.
Association with other diseases
The manifestation of signs of cervical osteochondrosis in men and women may be associated with other diseases. For example, experts have long established a connection between blood pressure and cervical osteochondrosis. This unpleasant disease is characterized by sharp drops in blood pressure throughout the day, and persistent hypertension is irrelevant for this disease.
An increase in pressure during osteochondrosis may be accompanied by pain in the arms, chest, legs and noise in the head. Signs of osteochondrosis of the cervical and thoracic at the same time include a decrease in the sensitivity of the skin in the collar zone. Constant stress and a long stay in an uncomfortable position can provoke a jump in blood pressure.
Dizziness and cervical osteochondrosis occur due to strong painful cerebral circulation, as well as due to the transmission of nerve signals. This can also occur due to existing problems regarding the vestibular apparatus. The initial signs of osteochondrosis of the cervical region include In this case, the patient does not feel rotating objects, but there is severe nausea. It is very difficult for the patient to be in a standing position.
It is important to note that during dizziness, it is necessary not only to visit a neuropathologist, but also to visit a ENT specialist so that this specialist excludes the presence of a pathological change in the nasopharynx.
In most cases, osteochondrosis is accompanied by a headache. It occurs due to vascular spasms, increased intracranial pressure, pinched nerve endings. The pain can manifest itself in different ways, whether it is dull or throbbing.
During osteochondrosis, headache attacks are similar to the sensations that occur with increased blood pressure, heart attack, angina pectoris and stroke.
Panic attacks can occur during osteochondrosis against the background of existing disorders in the cerebral circulation. The patient experiences physical discomfort and unreasonable fear. The duration of such an attack can be from several minutes to 1 hour. Attacks can be repeated several times a day. In addition, panic attacks are accompanied by incessant tears, a feeling of a heavy head, lethargy and apathy. If the patient has severe seizures, then it is necessary to regularly visit a psychiatrist and take tranquilizers.

Depression and fears arise with this disease against the background of constant pain, as well as a forced change in the usual way of life.
Diagnostic method
Most patients with osteochondrosis experience pain in the back of the head, in the arms and in the chest. Such a blurred picture of the disease greatly complicates the initial diagnosis. In addition, uncontrolled intake of painkillers hampers the timely diagnosis. A patient who does not experience pain feels completely healthy. As a result, people seek medical help too late, when irreversible processes are already beginning to develop in the tissues on the neck joints.
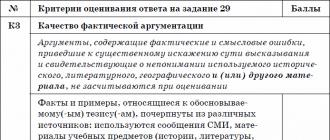
Diagnosis involves an x-ray, after which it will be possible to see r-signs of osteochondrosis of the cervical spine. After the x-ray, the patient is prescribed a course of treatment. With instability of r-signs of cervical osteochondrosis, the following symptoms will be observed:
- Angular deformity of affected segments.
- Displacement of the vertebrae to the side, back or forward.
- If within 2 vertebrae there are deviations on the vertical axis by more than 2 mm, then this indicates a pathology.
It is worth paying attention to the fact that radiography is an ineffective diagnostic method, especially at the last stage of development of osteochondrosis.
Also, during the diagnosis, magnetic resonance imaging can be assigned to the patient. MRI signs of osteochondrosis of the cervical spine help to establish a diagnosis for the patient. During tomography, a specialist can see bone structures, herniated discs, as well as their direction of development and size. If MR signs of osteochondrosis of the cervical spine are detected in time, then the disease can be quickly overcome.
No less effective solution than MRI is computed tomography. This procedure allows you to identify CT signs of osteochondrosis of the cervical spine. In addition, it is worth paying attention to the fact that computed tomography reveals the presence and size of a hernia much better.

Medical treatment
After the diagnosis, the specialist makes a diagnosis for the patient, and also prescribes the appropriate treatment. Treatment with medicines is aimed at combating pain, inflammation. Drug treatment can restore normal mobility and blood circulation. The main groups of drugs in the treatment of this disease are the following:
- Various analgesics in the form of injections and tablets to eliminate pain. Most often, "Diclofenac" or "Piroxicam" is prescribed for these purposes.
- Steroid and non-steroidal anti-inflammatory drugs, such as Dexamethasone or Prednisolone.
- Chondroprotectors that restore cartilage tissue. Basically, Chondroxide, Neurobeks, Teraflex are prescribed for these purposes.
- Muscle relaxants are prescribed to relax the muscles.
- Additionally, vitamin complexes are prescribed, which should contain all the vitamins of groups B, C, D, as well as ascorbic acid and retinol.
- For external use, you can use funds in the form of ointments, gels. The most effective are Nurofen and Voltaren, which improve blood circulation, relieve pain and spasms, anesthetize and warm.
You should also pay attention to the fact that those vitamins that are contained in the composition of food products will not be enough to treat this unpleasant disease. Therefore, you can use the complex preparation "Milgamma", which contains vitamins of group B, as well as "Lidocaine".
It is also recommended to take drugs that can improve cerebral circulation with existing cervical osteochondrosis. The intake of such funds is an obligatory component of the treatment of this disease. "Cavinton" and "Tanakan" are able to dilate blood vessels, as well as improve blood flow. "Piracetam" and "Ceraxon" are nootropic drugs that improve metabolic processes in the brain. In addition, these funds restore thinking and memory well.
Surgery
Surgical intervention for the treatment of osteochondrosis is used very rarely. However, the patient cannot do without surgery in cases where paralysis of the upper limbs is observed. Surgery will also be required if the patient has cerebral edema.
Complementary Therapy
As an additional therapeutic measure, massage is recommended. Also, experts in the complex advise using manual therapy in the form of jerky progressive movements. Very effective are: dosed traction, relaxing techniques and acupuncture.
Treatment at home
In combination with drug treatment, non-traditional recipes can also be used. Therapy at home involves the implementation of special exercises and techniques on a regular basis, the use of certain orthopedic devices. Prescriptions can be used as maintenance treatment traditional medicine.

To eliminate tension in the spine, reduce the load, strengthen the muscles of the neck, you can use the Shants collar. The neck and head are fixed in a certain position. Thanks to this, you can overcome insomnia, as well as prevent the development of pathological changes. This collar must be worn for several hours before going to bed. Under no circumstances should it be used all day.
With the help of self-massage, pain and spasms can be eliminated. And during this procedure, it is recommended to additionally rub the ointment, which can improve blood flow. Massage is done in a sitting position, the posture should be comfortable and relaxed. During it, stroking, circular rubbing are performed. When carrying out such a procedure, not only the neck is affected, but also the shoulder girdle.
It is important to note that with osteochondrosis of the cervical vertebra, it is forbidden to use any type of heating, with the exception of a sauna or a bath.
Taking special baths
You can get rid of soreness and inflammation with the help of therapeutic baths. Such procedures well help to relax the spine. Baths should be carried out every other day, and the course of treatment should include 15 to 20 procedures. Bath Recipes:
- Mix 300 g of mint and chamomile. Herbs brew 10 liters of boiling water. Let it brew for 2 hours, then filter.
- Take 40 g of lemon balm, the same amount of birch and mint leaves. The resulting composition brew 12 liters of boiling water, let it brew for 2 hours. After that, filter the broth, pour into the bath.
- To prepare an infusion based on sage, you need to take 300 g of this ingredient and 5 liters of boiling water. Let the medicinal solution brew for 2 hours, strain, after which it can be used.
For oral administration, you can use an infusion based on yarrow. Thanks to this, you can quickly get rid of inflammation, pain and spasms. To prepare the infusion, you need to take 230 ml of boiling water and 6 g of yarrow herb. Let the broth brew for an hour in a closed container. The finished product is taken three times a day, 15 ml.
Very effective in the fight against osteochondrosis is a solution consisting of 1 liter of water and 15 g of sea salt. The saline solution must be brought to a boil, after which it must cool completely. In the resulting composition, natural fabric is wetted, after which it is superimposed on the back of the neck.
Possible Complications
If the diagnosis was carried out in a timely manner, the treatment was correct, then the disease should proceed without any complications. Otherwise, rather severe pathological processes can develop, which in the future can provoke disability. Cervical osteochondrosis can be dangerous to human health. The main hazards include the following:
- Syndrome of the vertebral artery, in which there are organic and functional changes caused by impaired blood circulation in the brain.
- Arrhythmia and high blood pressure.
- Muscle atrophy in the upper limbs, weakness, numbness.
- The formation of a hernia, protrusion.
- neurological disorders.

Carrying out prevention
Preventive actions osteochondrosis involves the simplest actions, with the regular implementation of which you can prevent the occurrence of serious problems with your health. It is especially important to observe prevention for the elderly, as well as for those who spend too much time in a sitting position. To prevent the development of osteochondrosis, it is necessary:
- Take a hot shower every day for at least 10 minutes.
- Periodically go to the sauna, bath, to eliminate clamps in the neck and spasms.
- Sleep only on a special mattress and orthopedic pillow.
- When sedentary work, do at least 5 minutes of warm-up every hour.
To detect degenerative-dystrophic changes on the r-gram, it is necessary to carefully analyze the radiological signs. It will be possible to establish a diagnosis only after comparing the X-ray manifestations of the disease with each other and assessing the pathogenetic manifestations.
If degenerative-dystrophic processes are not treated in a timely manner, the disease progresses rapidly. Over time, the distance between the vertebrae decreases. Nerve root entrapment may occur. Because of this, pathological symptoms of the disease arise:, vertebral and.
What can be seen on the radiograph with osteochondrosis
It appears more often than in other areas. The condition occurs due to the anatomical features of the structure of the spinal column. Its lower sections account for the maximum load when lifting weights, performing physical exercises.
X-ray signs of osteochondrosis on an x-ray:
- narrowing of the intervertebral fissure;
- destruction of the endplates of the vertebrae with subchondral osteosclerosis;
- disc penetration into the vertebral body (Pommer's nodes);
- marginal growths along the corners of the vertebral bodies;
- compensatory reactions at increased load.
On the X-ray, you can detect the 2nd-4th degree of the disease. To identify the initial stage of pathology, the doctor must be highly qualified.

X-ray images (r-grams) do not show pinching of the nerves and hypertonicity of the muscles. The degree of severity of degenerative-dystrophic diseases of the spine on r-grams is determined by the degree of narrowing of the intervertebral discs, displacement of the vertebrae back and forth, instability of the vertebral segments.
Signs of spinal instability on x-ray
Spinal instability on r-images is determined by the following symptoms:
- hypermobility;
- instability;
- hypomobility.
Hypermobility is characterized by excessive displacement of a vertebra in the affected segment of the spinal column. In addition to displacement in pathology, the height of the intervertebral fissure may decrease. In the initial stages of the disease, it is reduced by about one-fourth.
It is better to assess this condition on radiographs with maximum extension and flexion of the spinal axis (functional tests). At the same time, the state of adjacent vertebrae and the posterior sections of the spinal canal is disturbed.
Hypomobility is characterized by a decrease in the distance between adjacent segments with minimal (than normal) movement of the vertebrae during functional tests (maximum flexion and extension). Osteochondrosis on the r-image is manifested by a change in the height of the intervertebral discs.
Extension or flexion is accompanied by adynamia of the motor segment of the spinal column against the background of degenerative-dystrophic changes in the spine.
With instability, radiological signs are characterized by the following symptoms:
- displacement of the vertebrae back and forth and to the sides;
- angular deformation of the affected segment;
- within two vertebrae, a deviation in the vertical axis of more than 2 mm is a variant of the pathology;
- in children, increased mobility can be observed in the C2 segment, therefore, when a difference in the segment of 2 mm is obtained on r-images in children, one cannot speak of pathological symptoms.
The manifestation of instability may be a sign of degenerative-dystrophic changes in the spinal column, but this is not always the case. For example, radiological signs of hyper- and hypomobility can be after traumatic injuries of the spine.
A sedentary lifestyle is the everyday life of a modern person. The child spends most of the time at the desk in the classroom. An adult man sits in a car, at an office desk. At home, a lot of time is spent in front of a computer or TV. As a result of this lifestyle, back pain begins to bother, posture becomes stooped. This is how signs of osteochondrosis appear, significantly reducing the flexibility of the spine. Unfortunately, many do not pay attention to the development of pathology. After a certain time, they face severe pain and loss of mobility.
Causes of the disease
Pathology causes ossification of cartilage. As a result of the deposition of calcium salts and the growth of connective tissue, there is a violation of the supply of nutrients to the body. The musculoskeletal system (ODA) begins to collapse. This pathology in medicine is called "osteochondrosis".
The causes of the development of the disease are hidden in numerous predisposing factors. The main ones are:
- spinal injuries (dislocations, fractures, bruises);
- obesity, overweight;
- foot pathology (clubfoot, flat feet, hallux valgus);
- age-related changes;
- wearing uncomfortable, tight shoes;
- hypodynamia;
- disturbed metabolism;
- a sharp refusal of athletes from training;
- curved spine (scoliosis, kyphosis, lordosis);
- professional features (jerks, weight lifting, uncomfortable posture);
- stress;
- prolonged and frequent hypothermia;
- specific climate (high humidity, low temperature).
It should be understood that pathology is not an age-related disease. Indeed, even in childhood, osteochondrosis is diagnosed.
The reasons for the development of the disease in babies, in addition to sitting for hours at a desk and computer, can be hidden in:
- hormonal problems;
- endocrine disorders;
- pathologies of the vascular system;
- various inflammations.

Classification of pathology
Depending on which department the signs of osteochondrosis are diagnosed, the disease can be:
- Cervical. This pathology often develops in people older than 40 years. However, there are cases of diagnosing the disease in patients aged 16 years. Among all musculoskeletal diseases, pathology occupies approximately 9%. Patients experience neck, headaches with osteochondrosis.
- thoracic. This type of pathology is more common in women. According to statistics, thoracic osteochondrosis is detected in almost 17% of all patients suffering from diseases of the musculoskeletal system. The disease is characterized by the occurrence of pain discomfort in the region of the heart.
- Lumbar. This is the most common ailment. Its share among ODA diseases is about 55%. Most often, lumbar osteochondrosis occurs in men. The symptoms of pathology are numerous. A characteristic manifestation of the disease is aching pain in the lower back.
- Sacral. This pathology is not common. Among ODA diseases, it occupies up to 7%. In women, a similar problem is diagnosed 2-3 times more often than in men. The disease develops in people over 60 years of age.
Stages of the disease
In medicine, another classification is common that allows you to determine the degree of osteochondrosis:

Symptoms of cervical pathology
The sensations experienced by the patient are completely dependent on the department in which osteochondrosis of the spine has developed.
Symptoms that indicate a lesion of the cervical region are as follows:
- dizziness;
- loss of visual acuity;
- hearing loss, ringing in the ears;
- the appearance before the eyes of colored spots, "flies";
- loss of consciousness;
- headache, localized in the parietal, temporal part or the back of the head, significantly aggravated when moving the neck;
- weakening or hoarseness of the voice, snoring;
- tooth decay;
- loss and numbness of the sensitivity of the hands, neck, face;
- pressure surges.
Signs of pathology in the thoracic region
This osteochondrosis of the spine manifests itself somewhat differently. The symptoms that characterize lesions of the thoracic region are as follows:
- Pain in the region of the heart. They can last a long time. Often they are oppressive, aching in nature. But sometimes there are sharp, stabbing, sharp. The patient is easily able to show the specific location of the pain.
- Numbness of the skin surface in the abdomen, chest, back.
- Severe pain in the region of the spine. Such signs of osteochondrosis are especially noticeable between the shoulder blades.
- Raising your arms causes severe pain.
- During a deep breath, there may be a sharp discomfort. Over time, it appears during exhalation.
- Leaning in any direction is difficult. The patient feels pain during such movements.

Symptoms of disorders in the lumbar region
Such a pathology, as noted above, is very common, which is not surprising. A sedentary lifestyle, weight lifting often provoke lumbar osteochondrosis.
Symptoms of this pathology:
- Pain is localized in the lumbar region. They are whining. Sudden movements, changes in body position or a long stay in one position significantly increase discomfort. The pain is reduced during the horizontal position.
- Stitching discomfort extends to the buttocks. As a rule, it is localized on one side. Sharp movement, sneezing, coughing increase the pain. Discomfort is reduced during the adoption of the “on all fours” position, when lying on the healthy side.
- Pathology often begins with a backache in the lumbar region. Such symptoms appear suddenly, with a sharp inclination, lifting of weight or extension of the body. An unpleasant state can last for several days. The discomfort is so intense that the person is unable to move.
- Atrophic changes in the hips and buttocks are observed.
- The skin is cold to the touch. The patient is faced with numbness in the buttocks, lower back.
- Sweating is disturbed.
- There is peeling, dryness, blue integument of the skin.
- Urination may be disturbed.
- Erectile dysfunction develops.
Symptoms of the pathology of the sacral region
In this case, the following signs of osteochondrosis are observed:
- Aching pulling pains cover the lower limbs. They are localized in the region of the lower leg, thighs. When moving, walking or staying in one position for a long time, the discomfort increases.
- The legs undergo atrophic changes. There is weakness in the lower extremities.
- There is numbness in the legs, coldness. The integuments of the skin acquire a bluish tint.
- Sweating in the legs is disturbed. They start to peel off. Dryness of the skin is noted.

Medical treatment
Drug treatment is prescribed during an exacerbation. Drugs can reduce unpleasant symptoms and affect some factors in the development of pathology.
The main groups of medicines used for osteochondrosis are:
- NSAIDs. They have an analgesic anti-inflammatory effect. Reduce the temperature in damaged tissues. Able to eliminate headaches in osteochondrosis. The most effective drugs are Dicloberl, Baralgin, Movalis, Nimid, Pentalgin, Nurofen. Along with injections and tablets, creams and ointments are used. Demanded means are "Nurofen", "Diclofenac", "Nimulid".
- Muscle relaxants. They perfectly relieve increased muscle tone. The following drugs are most often prescribed: Mydocalm, Baclofen, Sirdalud.
- Chondroprotectors. Medicines help reduce the destructive processes in cartilage. Their effect is aimed at restoring damaged tissues. The most popular are the medicines "Mukosat", "Arteparon", "Chondroxide", "Struktum".
Physiotherapy treatment
The doctor, explaining how to cure osteochondrosis, will definitely prescribe certain procedures to the patient. Physiotherapy treatment in combination with medications will significantly speed up recovery. In addition, it can prolong the period of remission.

There are many physiotherapeutic methods, and many of them cause a favorable effect in osteochondrosis:
- electrophoresis;
- acupuncture;
- magnetotherapy;
- massage;
- manual therapy;
- laser therapy;
- spinal traction;
- mud treatment;
- thermotherapy.
The patient may be prescribed one physiotherapy procedure or a set of measures. This is determined by the doctor based on the severity of the pathology and concomitant diseases.
Charging for the cervical region
The main reasons for the development of pathology lie in low mobility. Therefore, to combat the disease, the patient must be prescribed gymnastics for cervical osteochondrosis.
It allows you to normalize the mobility of the vertebrae, train muscle tissue, shoulder ligaments. The exercise therapy complex is selected for the patient, taking into account his pathology.
Gymnastics for cervical osteochondrosis is based on the following exercises:
- Tilts and turns of the head.
- Emphasis exercise. The head should be tilted forward. The open palm of the hand rests on the forehead. There is opposition. The head tends to go down, the hand tries to return it to its normal position. In this state, you should linger for 5-10 seconds, maintaining the tension of the neck muscles. Then relax. The same inclinations are made to the sides.
- Lying on the stomach, head lifts are carried out. Look up and forward. This exercise is repeated on the back.
- Try to reach the navel area with your chin. At the same time, move it along the sternum down. Pull the back of your head back in the same way.
Complex for the chest area
Charging for osteochondrosis includes the following exercises:
- Shoulder lifts, rotation.
- Waves with hands, circular movements. Crossing the upper limbs in front of you. Shaking hands.
- Lying on your stomach (back), lift your torso. Only the chest and shoulders should be lifted off the floor. The abdomen and legs are motionless.
- Pushups.

Gymnastics for the lumbosacral region
Charging with osteochondrosis is aimed at unloading the affected area by stretching. Such gymnastics trains the muscles of the press, back.
The exercise therapy complex contains the following exercises:
- Tilts in different directions.
- Pelvic rotation. There are circular movements. The pelvis extends in different directions.
- Body twists. It is necessary to strive to look back as deeply as possible.
- Lying on your stomach, you should bend as much as possible. Arms and legs rise above the floor for 15-20 seconds.
- Lying on your back, make straight leg lifts 45 degrees above the floor.
- Exercise "mill". The body leans parallel to the floor. Hands spread out to the sides should alternately reach the toes. The body rotates.
- Download the press. Lying on your back, raise and lower your torso. During the exercise, the legs should be bent at the knees.
- Sit on the floor. Place your hands on the surface. Raise your pelvis and try to hold it for a while.
- Lying on your stomach, lift your body. Feet must be fixed on the floor. Raising and lowering the torso, clasp your hands behind your head.
Prevention of osteochondrosis
Is it possible to protect your body from the development of an unpleasant pathology? Doctors say that it is quite real. For such purposes, they developed special rules to ensure the prevention of osteochondrosis.
- Sit correctly. When sitting, you should change position frequently. Staying in one position for more than 25 minutes is undesirable. If you are forced to sit all day, then from time to time you should get up and walk around the room.
- Stand right. This is true for many people who, by the nature of their activities, are forced to spend a long time on their feet. To protect your spine from the development of osteochondrosis, doctors recommend that you change your position every 20 minutes. If this is acceptable, it is better to change the type of activity. For example, after washing dishes, move on to ironing clothes.
- Lie down correctly. In this case, you need to choose the right mattress. Doctors do not recommend sleeping on bare hard boards or soft featherbeds. The best option is a special orthopedic mattress. It will significantly improve posture and protect against the development of osteochondrosis. Orthopedic mattresses allow you to completely relax and straighten your spine.
It is very important not to forget about the correct weight lifting. Sharp jerks often lead to an exacerbation of the pathology. Be sure to pay attention to exercise. In this case, no osteochondrosis will be terrible for you.
Our spine resembles a pearl necklace - the vertebrae, like pearls, are connected to each other with the help of rigid ligaments. Between the vertebrae are cartilaginous intervertebral discs that prevent the vertebrae from touching and play the role of shock absorbers between them. The spine usually consists of 32-34 vertebrae, which perform different tasks and belong to different parts of the spine. In total, five sections are distinguished in the spine:
- the cervical region, which consists of seven vertebrae;
- the thoracic region, which consists of twelve vertebrae;
- the lumbar region, which consists of five vertebrae;
- the sacral region, which consists of five vertebrae;
- coccygeal department, which consists of three to five vertebrae.
Inside the spinal column is the spinal canal - a cavity that is formed by the arches of the vertebrae. Nerve roots, blood vessels and the spinal cord pass through the spinal canal.
The human spine is adapted for upright posture, but upright posture is the factor that has a detrimental effect on our spine. The intervertebral cartilage is daily under enormous stress from human movements and the vibration that occurs during movement. Over time, the cartilage deforms and ceases to perform its functions in full. A person begins to experience tension and back pain - characteristic signs of osteochondrosis.
Diseases of the spine
Back pain is experienced by a huge number of people, and, regardless of age. Over 80% of people have experienced back pain at least once in their lives. Already at the age of 40-45, diseases of the spine become one of the most common causes of disability. The cause of various diseases of the spine is a violation of the anatomical shape and functional state of the spinal column. And such violations are caused by the way of life of a modern person. Using the achievements of civilization, humanity leads a sedentary lifestyle. Most people do not need to make muscle efforts, many people have an unbalanced diet, almost everyone is prone to bad habits. All this leads to degenerative and dystrophic changes in the vertebrae and intervertebral discs. Depending on what kind of changes have occurred, this or that disease occurs. Basically, all diseases of the spine have similar symptoms - pain and muscle tension, only the localization of pain differs. But it is osteochondrosis that is the most common disease - in 90% of cases it causes back pain.
Clinical picture of osteochondrosis
Osteochondrosis is a disease caused by a change in the intervertebral cartilage (chondron - means cartilage) with a concomitant reaction of the vertebral body (osteon - bone). When deformed, the intervertebral disc thickens and becomes thinner. In this case, the bone structure of the vertebral bodies is compressed, the vertebrae begin to experience overload. Pressed intervertebral discs are deformed even more, in some places they begin to protrude beyond the boundaries of the spine. Sooner or later, the disc compresses the nerve roots, which causes them to become inflamed. So there is a pain syndrome.
Depending on which part of the spine is damaged, there are several various kinds osteochondrosis. There are osteochondrosis cervical, thoracic, lumbar, sacral, widespread (when the lesion covers all parts of the spine). The most common are lumbar (more than 50% of diseases) and cervical (more than 25%) osteochondrosis. Often there are cases when several parts of the spine are affected - cervicothoracic osteochondrosis, lumbosacral.
The initial signs of osteochondrosis of the spine are manifested by the occurrence of dull pain and aches in the lower back (with lumbar osteochondrosis), uncomfortable tension in the muscles of the neck, and a crunch in the cervical vertebrae (with cervical osteochondrosis). Often, the pain that occurs with thoracic osteochondrosis is perceived by patients as pain in the heart.
In the future, pain often begins to radiate to the legs or arms; limbs become numb and cold. Often the pain appears even in the fingers or toes. Back pain is aggravated by sudden movements or shaking (for example, while traveling in transport). It becomes impossible to perform any work with the body tilted forward - with a bent back, the pain increases dramatically, but the patient does not always succeed in moving to a vertical position.
The more osteochondrosis develops, the more limited the mobility and flexibility of the spine. Thinning intervertebral discs reduce the distance between the vertebrae, and the latter have less room to move. In addition, the muscles around the affected area of the spine are constantly in a tense state - the body tries to block the damaged vertebrae to prevent their further deformation. "Clamped muscles" deliver additional discomfort and pain, and contribute to further greater restriction mobility.
All of these symptoms can occur both at rest and during movement or physical effort (there is additional pressure on the nerve roots).
Diagnosis of osteochondrosis
How is osteochondrosis identified if its symptoms at the initial stage can be mistaken for symptoms of other diseases?
Of course, the doctor will be interested in the anamnesis. After listening to the patient and conducting an examination, the doctor will send him for an additional examination. There are several different examination methods for diagnosing osteochondrosis.
Radiography
Examination of the spine using x-rays (spondylography) allows you to objectively assess its condition. X-ray signs of osteochondrosis are detected already at the initial stages of the disease. Spondylography gives an idea of the state of the vertebrae and, indirectly, of the state of the bone canals and intervertebral discs. Pictures are taken in frontal and lateral projection. If the doctor deems it necessary, functional images are assigned in various positions - in the position of lateral tilts, in the position of flexion and extension.
If necessary, the patient is given a tomogram - a layered x-ray examination. In addition to the usual x-ray examination, for special indications, contrast x-ray examinations of the spine are used. Such surveys include:
- Pneumomyelography - using 20 to 40 milliliters of air as a contrast. Air is introduced into the spinal canal after a lumbar puncture;
- Angiography - when 10-15 milliliters of contrast is injected into the vertebral or carotid artery, and then a series of pictures is taken in two projections;
- Myelography uses a dye injected into the spine to highlight the structure of the spine. With the help of myelography, you can determine the force of pressure of the intervertebral disc on the spinal cord. The procedure takes about half an hour and is performed under local anesthesia. First, the lower back is injected with an anesthetic. Then, using a thin needle, a coloring opaque substance is injected into the fluid that fills the space near the spinal cord. After injection of contrast, the x-ray table slowly tilts and the substance moves along the spine from the lower to the upper section. After the end of the procedure, the patient needs to lie down for several hours.
- Discography - carried out similarly to myelography, with the difference that a staining substance is injected into a painful disc to determine whether it is the cause of osteochondrosis.
Other methods of examination of the spine
Radiography does not give the doctor a complete picture to establish an accurate diagnosis. With its help, one can reliably judge mainly the degree of deterioration of the vertebrae and their displacement. Unlike radiography, computed tomography gives a clear picture, which can be used to judge the presence and location of the intervertebral hernia. This method of examination allows you to get a clear and detailed image of the spinal column and shows all the changes in it from different positions and angles. At the same time, computed tomography is a more gentle method that is easily tolerated by patients.
Magnetic resonance imaging (MRI) - this method provides the most accurate image of the spine to date. This is possible due to the fact that the survey is not x-rays but with a strong magnetic field. MRI is the preferred method of examination, because it allows you to assess the condition of the spinal canal, nerve fibers, bones, muscles, ligaments; with it, you can see any changes that occur with osteochondrosis.

Symptoms of osteochondrosis
The localization and nature of pain in osteochondrosis depends on which part of the spine is affected. Of course, the signs of cervical osteochondrosis differ in many ways from the signs of a lesion, for example, in the lumbar spine. And yet, there are common symptoms of osteochondrosis that will tell you that you are sick:
- making a sharp movement, turning your head to failure, twisting the body in combination with a tilt, or quickly straightening up after a tilt - you suddenly feel a sharp and severe back pain that looks like an electric shock;
- after the "shock" you are paralyzed for some time and freeze, unable to move;
- the muscles in the place where the pain arose are painfully tense;
- if you press your fingers in the place of the spine where you felt pain, then the feeling of sharp pain will repeat;
- spinal mobility becomes markedly limited. It is difficult for you to find a position in which the pain could subside;
- if the posture adopted by you is unsuccessful, the pain increases dramatically.
There are also symptoms that are characteristic of a certain type of osteochondrosis.
Cervical osteochondrosis
Signs of cervical osteochondrosis are easily confused with symptoms of other diseases. . When the cervical region is affected in the spine, the pain is transmitted to the arms, the back of the head; severe headaches develop into migraines.
There may be severe, boring pain in the neck or occiput, which is aggravated by turning the head, coughing, sneezing. Neck pain can radiate to the shoulder and to the side of the chest.
In some cases, the patient experiences not only a headache, but also dizziness, tinnitus, visual disturbances. In the case of progression of the disease, a persistent violation of the blood circulation of the brain or spinal cord is possible.
With compression (squeezing) of the nerve roots in the lower segments of the cervical region, symptoms similar to those of angina pectoris occur - pain in the region of the heart, neck, and shoulder blades. The pain is aggravated by movement and is not relieved by cardiac drugs.
The causes of osteochondrosis of the cervical spine are due to the anatomical features of this segment of the spine. The cervical vertebrae experience a constant load, holding and often turning the head, while the size of the vertebrae of the cervical region is significantly smaller than the vertebrae of the rest of the spine. We must not forget about the narrowness of the internal spinal canal.
A huge number of nerves and blood vessels are concentrated in the neck area, including a large vertebral artery passing inside the spinal canal, which feeds the brain. All this fits snugly together in the cramped space of the cervical vertebrae. With cervical osteochondrosis with a displacement of the vertebrae, the nerve root is infringed, its edema and inflammation quickly develop.
Osteochondrosis of the thoracic and lumbar
The spine in the thoracic region, together with the ribs, serves as a framework that protects the vital organs. The thoracic vertebrae have such a structure, due to which they remain inactive, so they rarely undergo degradation and deformation. As a result, pain in the thoracic spine is also rare. Signs of osteochondrosis of the thoracic region are often mistaken for manifestations of other diseases - it is confused with angina pectoris and even mistaken for myocardial infarction.
When the thoracic spine is affected, the pain is girdle in nature, and it may seem to the patient that it comes from the lungs, heart, or even stomach. It is precisely because the signs of thoracic osteochondrosis are “disguised” as other diseases that differential diagnosis is of great importance in making a diagnosis.
Lumbar osteochondrosis is nothing more than changes in the intervertebral discs located, respectively, in the lumbar region, which consists of 5 large vertebrae. The lumbar region connects the sacrum and the thoracic region. Osteochondrosis of the lumbar spine occurs much more often than other types of osteochondrosis.
This fact is explained by the fact that it is on the lumbar spine of a person that the entire load of the human body weight, as well as the load that modern man have to be carried daily - briefcases, shopping bags, and so on. That is why so often patients go to the doctor not only with osteochondrosis itself, but also with the complications that it entails, in particular, with intervertebral hernias. Intervertebral hernia is not such a harmless phenomenon; in especially severe cases, even paralysis of the limbs is possible.
Symptoms of lumbar osteochondrosis
People whose doctor has diagnosed the presence of lumbar osteochondrosis note the following complaints and symptoms:
- Pain in the lumbar region, and the pain is sometimes shooting in nature and gives to the buttocks and legs. Pain when bending or squatting a sick person increases significantly. The same thing happens with a long stay in an uncomfortable position, or sneezing, coughing and physical exertion.
- Feeling of numbness in the legs, especially toes.
- Violation of the full functioning of the genital organs, often women have mild urinary incontinence.
Causes of lumbar osteochondrosis
Osteochondrosis of the lumbar causes is quite specific. Doctors call the upright posture of a person the cause of the disease. However, of course, if this were the main and only cause of the disease, all people would be ill without exception. But in fact, the disease develops only in the presence of certain provoking factors. Doctors cite the following factors:
- Violation of normal metabolism.
- The presence of hypodynamia in a person.
- Excess body weight of a sick person.
- Systematic excessive physical activity, especially associated with weight lifting.
The cause of intense pain in osteochondrosis is the pinching of the nerve roots. This pinching occurs due to the fact that the intervertebral disc protrudes, but the gaps between the vertebrae, on the contrary, are significantly narrowed.
The core of the disk gradually dries out and deforms, respectively, the ability to depreciate significantly deteriorates.
Treatment of lumbar osteochondrosis
Osteochondrosis of the lumbar spine, like any other disease, needs long-term and intensive complex treatment. It is especially difficult to treat a complex and advanced form of the disease, aggravated by the presence of numerous hernias.
Treatment of lumbar osteochondrosis should be prescribed only by a qualified specialist. After a preliminary examination, the doctor, based on the data obtained and the individual characteristics of each individual patient, will prescribe the most suitable treatment for him. Modern methods of treatment of osteochondrosis allow you to find an individual approach to each person.
As a rule, the treatment of osteochondrosis of the lumbar spine is as follows:
- Acupuncture procedure.
- Comprehensive massage, including acupressure.
- Various types of heating - salt, UHF and electrophoresis.
- Pharmacological preparations aimed at restoring cartilage tissue.
The main objective of these procedures is to restore full blood circulation and eliminate congestion and inflammation in the lumbar region. It is also very important to relieve swelling of blood vessels, restore the normal metabolic process in the intervertebral discs, thereby stimulating the start of the process of natural restoration of cartilage tissue. It is also very important to remove the muscle spasms associated with osteochondrosis of the lumbar region.

Measures and means of prevention of osteochondrosis
It is also very important to know how to prevent the occurrence of osteochondrosis of the lumbar. Prevention of the disease will help to avoid many unpleasant minutes associated with the presence of the disease, its diagnosis and subsequent treatment. And, of course, we must not forget that. That prevention is much cheaper than treating an already developed disease.
Properly selected diet
Nutrition is extremely important for the normal functioning of all systems of the human body. Was no exception and lumbar osteochondrosis. A special diet is not only an excellent preventive measure, but also helps to alleviate the condition of a disease already present in a person, thereby increasing the effectiveness of treatment.
The main condition for a properly composed diet for a person suffering from any disease of the spine, including osteochondrosis of the lumbar spine, is a salt-free diet. The menu of a sick person should include foods such as vegetables, fruits, lean meats. It is extremely important to completely eliminate all fatty, spicy and fried foods, spices, salt and sugar from the diet. From drinks it is worth giving preference to tea, a decoction of wild rose and lingonberries. Completely eliminate the use of coffee, carbonated and alcoholic beverages.
Proper lying position and bed selection
To prevent the onset of the disease and successful treatment, it is very important to know how to lie correctly and, most importantly, on what. The best choice would be a flat and moderately hard bed. Do not fall into fanaticism and try to sleep on the boards. It is much more reasonable to cover the bed with a thin shield made of wooden boards, on top of which it is necessary to lay a thin mattress. In the event that a suitable mattress is not at hand, you can use several thin woolen blankets instead.
This measure is necessary in order for the back to restore its physiological shape, and for the subluxations of the vertebrae to straighten out. However, be prepared for the fact that at first you will experience quite intense pain, which will continue until the vertebrae return to their normal position. To alleviate this condition, at first, you can put a cotton pad under the painful joint. Thus, you relieve muscle tension and slightly ease the pain.
A lot of people suffering from lumbar osteochondrosis make the same mistake - they go to bed on their backs. However, in this case, it would be much more reasonable to lie down to sleep on your stomach, pulling your leg bent at the knee under your chest. Under the stomach, you can put a flat thin pillow. And only after lying in this position for at least half an hour, you can very carefully turn on your back, put your hands behind your head, fully stretch your legs and spread them with your socks in different directions. In the event that the pain is too strong and it is not possible to do all the above steps, perform them exactly as much as you can. Each time you will get better and better.
In the morning, after waking up, getting out of bed for a person suffering from osteochondrosis is extremely difficult and often painful. In order to facilitate this process, doctors recommend the following. After you wake up, turn on your back, stretch both your arms and legs several times. After that, start very gently moving your feet in a clockwise direction. After that, carefully turn onto your stomach, stretch again and very carefully lower your legs alternately to the floor. After that, transfer the weight to your legs, leaning on your hands. Get up also very carefully, without making sudden movements.
It is equally important to sit correctly
Indeed, in the event that a person sits incorrectly, the severity is distributed unevenly and has an extremely negative effect on the spinal column. In order to prevent this from happening, the human body should not rest on the lower back or coccyx, but on the buttocks, which, in fact, are intended for this. However, this is possible only in one case - if a person sits on a hard surface. It is also very important to choose the right height of the chair - it must correspond to the length of the lower leg. Improper sitting is also included in the main causes of exacerbation of osteochondrosis.
In the event that at work you are forced to spend a long amount of time sitting, turn the body in both directions every half hour. Also be sure to do five circular rotations, both with the neck and with the shoulders. Make sure that your shoulders are as deployed as possible, and try to keep your head as straight as possible.
The seat behind the wheel deserves no less close attention. The back should have full support. Buy a special roller, which must be constantly laid between the back of the seat and the lower back. Keep your back and head straight while riding. Do not drive for more than 3 consecutive hours. Be sure to make regular stops. Get out of the car and do simple physical exercises such as raising and lowering your arms, squatting, turning and bending over. In the end, even just walking around the car can have a positive effect on the condition of the spine and muscular system. The same goes for watching TV or reading. The most important rule - do not linger for a long time in the same static position - this has an extremely negative effect on the condition of the spine.
Many people try to use folk methods for the treatment of osteochondrosis. However, this is still not worth doing, since the spine is too serious and complex a phenomenon. And in no case should you experiment, wondering if this or that traditional medicine recipe will help. After all, in case of failure, the price of a mistake will be too high. At best, there will simply be no improvement. And at worst, a person can pay for a mistake with the ability to walk.