Cervicitis - what is it? Diagnosis, causes, treatment. Cervicitis in women - inflammation of the cervix Can cervicitis develop from inflammation of the cyst
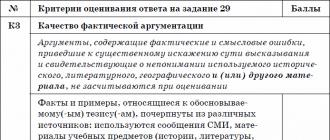
Gynecologists attribute cervicitis, an inflammatory process that affects the cervix, to fairly common diseases of the female genital area, because 50% of women suffer it at least once throughout their lives.
The cervix becomes infected, which serves as a protective barrier for infectious microorganisms, inflammation occurs, which is divided into several stages. Moreover, in two-thirds of cases, this disease occurs in the reproductive age.
Causes of inflammation
Given the fact that the disease is quite common, it can be caused by many reasons.
We list the main ones:
- vaginal infections or sexually transmitted diseases- (chlamydia, gonorrhea, trichomoniasis, etc.);
- candidiasis;
- herpes simplex virus- (genital herpes);
- human papillomavirus;
- birth injury of the cervix- mechanical damage resulting from unprofessional abortion, diagnostic curettage of the uterus, artificial expansion of the cervix using special tools, or installation or removal of the contraceptive coil;
- early onset of sexual activity promiscuity, the presence of several sexual partners;
- non-compliance with the rules of personal hygiene -(for example, a forgotten tampon can cause irritation of the cervix and inflammation, improper washing - from the anus towards the vagina - often leads to infection with Escherichia coli);
- allergic reaction to latex or spermicidal formulations, etc..
Symptoms and signs
The first symptom of cervicitis may be more intense vaginal discharge, which begins immediately after the end of menstruation. However, due to the weak severity, it is quite difficult to detect the disease without a gynecological examination at this stage.
The main symptoms include the following:
- itching, burning of the external genital organs and their redness;
- burning or stinging when urinating;
- copious discharge;
- bleeding between periods;
- painful intercourse;
- small spotting or even bleeding immediately after intercourse;
- pain in the lower abdomen or lower back (sometimes they appear only during intercourse);
- mild nausea, fever, dizziness and pronounced pain in the lower abdomen (occur when the infection spreads);
- hyperemia and swelling of the external opening of the cervical canal, accompanied by protrusion of the uterine mucosa and small hemorrhages or ulcerations (detected during examination).
It should be noted that depending on the type of pathogen and the general state of immunity, cervicitis can have various manifestations. So, for example, cervicitis caused by gonorrhea usually proceeds acutely, its signs are pronounced. On the other hand, the symptoms of chlamydial infection are less noticeable.
For cervicitis, which arose against the background of herpes, a loose, bright red cervix with ulcerations is characteristic. In the presence of trichomoniasis, the disease is manifested by small hemorrhages on the cervix and the presence of atypical cells in the smear. The human papillomavirus against the background of cervicitis often leads to the formation of genital warts and extensive ulceration of the cervix.
Cervicitis is dangerous because with a mild stage of the disease, its course can be completely invisible. And if in an acute form it was not detected and, as a result, not cured, then the disease passes into a protracted chronic stage. In chronic cervicitis, the main signs of inflammation (edema and hyperemia) are less pronounced.
However, if left untreated, and in the future, inflammation will begin to spread to the tissues and glands surrounding the cervix, as a result of which cysts and infiltrates will begin to form, and the cervix will thicken. Therefore, do not neglect regular visits to the doctor, because this is extremely important for your health and the ability to become pregnant and give birth to a healthy baby.
Separately, I would like to say about the discharge from the urethra or vagina with cervicitis, because, depending on their nature, one can also judge the causative agent of the disease. So, for example, with cervicitis against the background of gonorrhea, the discharge, as a rule, becomes yellow with an admixture of pus.
With chlamydia or mycoplasmosis, changes in secretions are less pronounced. Usually they are transparent or white in color, a shade of yellowness may be present. If the cause of cervicitis is urogenital trichomoniasis, then the discharge will be frothy. And if the case is in candidiasis, then the discharge is similar to the discharge with thrush. They are white in color and have a creamy texture.
Varieties of infection
Cervicitis has some varieties. Let's talk about each of them.
Spicy
This type of disease is characterized by rapid development. Infectious and inflammatory processes are pronounced, in addition, almost all symptoms of the disease can often be present at the same time.
Chronic
It can occur against the background of other inflammatory diseases or develop from untreated acute cervicitis.
Usually chronic cervicitis accompanied by meager mucopurulent or simply mucous secretions, slight swelling of the tissues of the cervix.
In the case of a long course of the chronic stage of cervicitis, the cervix begins to thicken, and erosion often occurs.
Purulent
Based on the name, it is clear that in this case the inflammation is accompanied by abundant mucopurulent discharge.
The cause of their occurrence may be male urethritis caused by sexually transmitted diseases. Most often, this type of cervicitis occurs when a patient has gonorrhea.
atrophic
With atrophic cervicitis, inflammation is accompanied by thinning of the tissues of the cervix. In the case of advanced forms of atrophy of different parts of the genital tract, there is often a violation of urination, therefore, in addition to the gynecologist, it is imperative to visit a urologist. Most often, this type of disease develops from a chronic form.
Viral
Caused by diseases of viral etiology (human papillomavirus or genital herpes). Its treatment, as a rule, is complex and rather difficult: a woman is prescribed antiviral drugs, immunomodulators, and irrigation of the uterine cavity with special formulations is also necessary.
Bacterial
With bacterial cervicitis, a strong inflammatory reaction is not observed, although there is still a violation of the vaginal microflora. It can be caused by a bacterial infection - colpitis, gonorrhea, vaginosis, etc.
cystic
The most unpleasant type of cervicitis. Its cause is considered a combination of several infections (streptococci, staphylococci, trichomonas, chlamydia, etc.). The result of such a "bouquet" of diseases is the growth of cylindrical epithelium on the surface of the uterus and its complete overgrowth with cysts.
According to experts, in this case, the cervix is an unpleasant sight, because it is almost completely covered with countless cysts. Often combined with erosion.
Nonspecific cervicitis
This species is not associated with any sexually transmitted infections. Most often occurs in the presence of bacterial vaginosis. Nonspecific cervicitis occurs, as a rule, in young women and is characterized by fairly abundant purulent discharge. Moreover, as in other cases, inflammation begins due to a violation of the natural microflora of the vagina.
How the disease is diagnosed
Cervicitis is often asymptomatic, so most often this disease is discovered by chance during routine physical examinations or when contacting a gynecologist for other diseases.
The essence of the diagnosis is to identify the causes of an inflamed infection, it is the definition of the pathogen that guarantees effective treatment.
An accurate diagnosis is established based on the results:
- examination with the help of gynecological mirrors of the surface of the cervix;
- extended colposcopy, which allows you to consider even minor changes in the epithelium of the cervix (vascular loops, swelling of the mucosa, ectopia or erosion, hyperemia and the nature of inflammation) and determine the effectiveness of further treatment based on this;
- laboratory studies (bacteria for sensitivity to antibiotics and microflora, smear, PCR diagnostics, pH-metry of the vaginal discharge, etc.);
- special diagnostic methods (enzymatic immunoassay, DNA probe, etc.).
Methods for the treatment of cervicitis
For a successful cure, first of all, it is necessary to determine the causative agent of the disease and eliminate it and predisposing factors (metabolic, hormonal, immune disorders). Therefore, the type of treatment for cervicitis largely depends on the cause of the disease.
After diagnosing and identifying the pathogen, the gynecologist will prescribe you a number of medications that are most effective and short term can fight the infection. Moreover, throughout the entire period of treatment, you will need to take laboratory tests and undergo colposcopy to monitor the dynamics of recovery.
It is also worth noting that in order to exclude the likelihood of re-infection, it is worthwhile to treat the sexual partner.
Treatment with candles
Candles from cervicitis, shown with its non-specific form, have an excellent healing effect. Influencing inflammation locally, they eliminate unpleasant secretions and restore disease-damaged tissue, while removing the affected one. The maximum effect can be achieved by combining candles with medical pads.
But remember that it is not recommended to use candles during pregnancy, during menstruation and a few days before it starts. Also, stop treatment with the use of suppositories and consult a doctor if pain, itching, redness or peeling of the external genitalia occurs.
Treatment with folk remedies
In addition to the main drug treatment, patients with cervicitis often use alternative methods.
Let's take a look at a few of them.
Decoction. In equal quantities, take raspberries, birch leaves, herbs of wormwood, St. John's wort, mint and horsetail and chop a little. Pour 5 g of the resulting mixture with a glass of boiling water and heat in a water bath for 10 minutes. Infuse the decoction for about an hour, then strain and take 3 times a day, a third of a glass every day 30 minutes before meals.
Infusion for douching. Take birch leaves, calendula flowers, motherwort herb, dandelion and licorice roots and cumin in equal amounts, chop everything and mix thoroughly. After that, pour 10 g of the resulting dry mixture into 500 ml of boiled water (preferably warm) and heat in a water bath for a quarter of an hour. Then leave the resulting broth for at least 2 hours in a warm place and strain. The solution for douching is ready. For each procedure, take 200 ml of infusion and repeat douching 3 times a day.
Ointment. Lilac flowers, snake mountaineer and dandelion root, fireweed and birch leaves, herbs of celandine, wormwood, St. John's wort and sage, as well as grind flax seeds. Take 50 g of the resulting dry mixture, pour 500 ml of water and boil over low heat until the volume of water decreases by about 2 times. Then add 50 g of butter and cook for another quarter of an hour.
After that, remove from heat, add 50 g of honey and stir. Lubricate the strip of bandage with the resulting ointment, forming a candle, and do not forget to leave the edge of the bandage free (about 5-7 cm) for easy removal. Insert the resulting candle into the vagina before going to bed.
Surgical methods of treatment
If you have chronic stage cervicitis and conservative treatment does not give a positive result, then most likely, in the absence of infections, the gynecologist will offer you one of the methods of surgical intervention, namely cryotherapy, diathermocoagulation or laser therapy.
Cervicitis, what is it? How to treat cervical cervicitis
The cervix is a kind of barrier, the task of which is to prevent the spread of infection by ascending through the uterus and its appendages. If her protective function is broken, then pathogens penetrate into the upper sections of the internal genital organs of a woman, provoking the development of cervicitis. A woman begins to be disturbed by discharge of an atypical nature, pain with localization in the lower abdomen is periodic or constant, which intensifies during intercourse or urination.
What it is?
Cervicitis is an inflammation of the cervix, in short, in simple terms. But, not everything is so simple - let's look at the issue in detail.
Causes of cervicitis
The main cause of cervicitis are diseases that are sexually transmitted. With the development of a certain sexually transmitted disease, thick mucus gradually thins, resulting in inflammation of the mucous membrane. After that, the infection begins to spread to the base of the cervix. In view of such changes, microbes gradually enter the uterus, appendages, and later spread to the bladder, kidneys and other organs. As a result, pathological phenomena develop in the pelvic cavity of a woman, up to peritonitis.
If sexually transmitted diseases are considered the main cause of the development of cervicitis in a woman, then doctors also identify a number of factors that contribute to the development of this disease. The risk of developing cervicitis increases significantly if a woman has been infected with the herpes virus or. Cervicitis can overtake a girl at a time when she is just starting an active sex life. Also, cervical cervicitis can manifest itself as a consequence of mechanical or chemical irritation (we are talking about contraceptives or hygiene products). In some cases, the inflammatory process occurs as a result of an allergic reaction of the body to latex, other components of contraceptives or personal care products.
A factor provoking the disease is also a weakened immune system due to other somatic diseases. In addition, cervicitis can develop as a result of injuries caused during an abortion or childbirth (in this case, it is important to suture all tears of the perineum and cervix obtained in the birth process with high quality). Also, the disease often affects women who have entered the menopause.
All the reasons described above contribute to the active reproduction of microorganisms classified as opportunistic pathogens (staphylococci, streptococci, enterococci, E. coli). In the normal state of health of a woman, such microorganisms are present in the microflora of the vagina.
Symptoms of cervicitis
Manifestations of the acute form of the disease are pronounced significantly. The patient is concerned about purulent or profuse mucous leucorrhoea, vaginal itching and burning, which are aggravated by urination. Pain in cervicitis may also bother. Usually these are dull or aching pains in the lower abdomen, painful intercourse. Other signs of the disease are due to concomitant pathology.
If the inflammatory process of the cervix has arisen against the background, frequent and painful urination worries. With an inflammatory process in the cervix, there is an increase in temperature from subfebrile (above 37) to febrile numbers (38 and above). With a combination of pseudo-erosion and cervicitis, spotting may appear after intercourse. A distinctive feature of the disease is the exacerbation of all clinical symptoms after menstruation.

Chronic inflammation of the cervix
A disease that has not been adequately and timely treated in the acute stage becomes chronic. Signs of chronic cervicitis are less pronounced or practically absent. The discharge becomes cloudy-mucous, the squamous epithelium of the vaginal part of the cervix is replaced by a cylindrical one from the cervical canal, pseudo-erosion of the cervix is formed.
Inflammatory phenomena (redness and swelling) are mild. With the spread of inflammation to the surrounding tissues and deep into, the neck thickens, it is possible to again replace the cylindrical epithelium with a flat one during ectopia, which is accompanied by the formation of naboth cysts and infiltrates.
Lymphocytic cervicitis
The disease is also called follicular cervicitis. This form of inflammation is asymptomatic and occurs in menopausal women. The process is a lymphoid "impregnation" of the walls of the cervix, resulting in the formation of follicular benign formations. If this form of inflammation is detected, the doctor will definitely conduct a differential diagnosis with malignant lymphosarcoma.
Candida cervicitis
Occurs in a situation where there is already a fungal infection in the vagina (). When examining the cervix, white plaques are determined in the mirrors, which are easily scraped off, as a result of which the inflamed red mucosa is exposed.
Viral cervicitis
The disease appears as a result of infection with the herpes simplex virus, human papilloma,. Represents a certain difficulty in recognition, since it does not have specific features. During the examination, the doctor may see vesicles characteristic of a herpes infection, or only a laboratory will confirm the diagnosis.
Cystic cervicitis
It is a form of the disease in which the formation of benign. As a result inflammatory process there is a blockage of the glands that secrete mucus and their subsequent growth, which the gynecologist will detect during examination or colposcopy.
Atrophic cervicitis
Most often it is a chronic and non-specific form of the disease. Frequent causes of atrophic inflammation are traumatic manipulations associated with a violation of the integrity of the cervical canal of the uterus or childbirth.
Diagnostics
The diagnosis is established by a gynecologist based on the results of the examination and additional research methods. He collects an anamnesis, studies complaints and symptoms. During the examination on the chair, the doctor sees foci of inflammation, pinpoint hemorrhages on the surface of the exocervix, an increase in its size due to swelling, redness and swelling of the walls of the vagina, external genitalia.
The gynecologist takes a smear from the surface of the cervix for further examination under a microscope - cytology. The resulting material is also sown on nutrient media - the grown colonies of the pathogen make it possible to determine its type and sensitivity to antibiotics. If necessary, the doctor measures the pH of the discharge from the vagina - its increase indicates changes in its microflora.
Chronic cervicitis leads to the appearance of pathological foci on the cervix - they are detected when treated with iodine solution. In this case, colposcopy is performed - the study of the exocervix epithelium under high magnification in order to exclude malignant degeneration of its cells. For the diagnosis of chronic endocervicitis, curettage of the cervical canal is performed, followed by a study of the cellular composition of the obtained material. To exclude tumors of the female reproductive system, they are examined using ultrasound.

Treatment of cervicitis
First of all, it is necessary to identify and eliminate the factors that could cause cervicitis. It is worth noting that if sexually transmitted infections are detected, the woman's sexual partner must also be treated.
The tactics of treating cervicitis depends on the identified cause of the disease. The treatment regimen for different types cervicitis:
- In case of fungal infection, antimycotics are used: inside Fluconazole, in the vagina - Natamycin tablets, suppositories with econazole;
- With chlamydial infection - a combination of several antibiotics (Tetracycline + Azithromycin) is prescribed for a period of at least 21 days;
- With atrophic inflammation, the introduction of suppositories, creams, gels containing estriol (Divigel) into the vagina helps;
- For bacterial infections - treatment with antibiotics (candles Neomycin, Metronidazole), combined anti-inflammatory and antibacterial drugs (Terzhinan). After sanitation, suppositories with useful lactobacilli are prescribed to restore normal microflora (Acilact).
After the acute stage of the disease subsides, it is possible to use local methods of treatment. Effective use of creams and suppositories (terzhinan). Treatment of the mucous membranes of the vagina and cervix with solutions of silver nitrate, chlorophyllipt or dimexide is recommended.
In advanced cases of the disease, when atrophic changes are observed in the mucous membrane of the cervix, local hormone therapy (Ovestin) is indicated, which promotes the regeneration of the epithelium and the restoration of the normal microflora of the vagina.
Conservative treatment may not give the desired results in the chronic stage of cervicitis. In such cases, the doctor may recommend surgical treatment (cryotherapy, laser therapy, diathermocoagulation).
To evaluate the effectiveness of treatment, a control colposcopy is performed and laboratory tests are performed.
The danger of cervicitis in pregnant women
Cervicitis is associated with the destruction of the mucous plug that protects the uterus from infection from the vagina. The likelihood of the disease and the transition of the inflammatory process into a chronic form increases due to the inevitable decrease in immunity during this period (this prevents fetal rejection).
In the presence of cervicitis in pregnant women, the risk of complications such as miscarriage and premature birth increases. Possible infection of the fetus, which leads to abnormal development, the appearance of deformities, intrauterine death, death of the newborn in the first months of life.
Cervicitis is a major threat early dates pregnancy, when organs and systems are formed in the fetus. Most often, a woman has a miscarriage. If acute cervicitis occurs in the middle or end of pregnancy, the child may develop hydrocephalus, kidney disease and other organs. Therefore, when planning a pregnancy, a woman should be cured of cervicitis in advance, strengthen her immune system. Treatment is mandatory, as the risk of complications is very high.
Content
A dangerous disease characterized by inflammation of the cervix worries many women. The disease can cause severe damage to the body. The disease is especially dangerous for pregnant women. It is important to know its signs and consult a doctor in time.
What is cervicitis
The disease is an inflammation of the cervical canal located in the cervix. Specialists distinguish between exocervicitis and endocervicitis. The first option is considered by doctors as an inflammatory disease of the cervix in the vaginal area. In the second case, the focus of the disease occurs on the inner membranes of the cervical canal. The occurrence of the disease can be caused by microorganisms:
The formation of chronic cervicitis in a woman's body is associated with the ingress of pathogenic microorganisms into the cervical region. If the treatment of a chronic course is not started on time, the disease can lead to the development of erosion of the uterine cervix, thickening of its walls. Microbes can arise inside due to several reasons:
- descent of the cervix or vagina;
- frequent sexual intercourse with different partners;
- incorrect regimen of hormonal contraceptives;
- violations of the rules of personal hygiene;
- the occurrence of inflammation in the organs of the reproductive system.
The disease in the chronic form is manifested by whitish discharge, having a mucous structure, swelling of the cervix. If there is a period of exacerbation, other symptoms may occur:
- itching in the genital area;
- pain during urination;
- burning in the vagina;
- pain of a pulling nature in the lower abdomen;
- specific vaginal discharge.
Acute cervicitis
The occurrence of acute cervicitis may be due to the appearance of inflammation due to the presence of microbes in the body. Symptoms of this form of the disease are:
- mucous discharge with a possible admixture of diffuse pus;
- increase in body temperature;
- pain in the lower abdomen of a dull nature;
- pain sensations in lumbar;
- discomfort during urination and frequent urge;
- hot flashes concentrated in the pelvic area.
The characteristic features of an acute inflammatory process may vary depending on the pathogen that caused it. If the disease is of a gonorrheal nature, the lesion affects the epithelium of the endocervical glands and spreads to the mucous membranes. If the culprits of the disease are staphylococci or streptococci, inflammation appears inside the gland, affecting the cervix. Gradually, the bacteria spread through the lymphatics and to other organs.
Atrophic cervicitis
A disease in which inflammation of the cervix occurs under the influence of advanced infections or the human papillomavirus is called atrophic cervicitis. Therapy for this form of the disease depends on the causes by which it is caused. The doctor prescribes hormonal preparations containing estrogen, which are designed to nourish the tissues. As maintenance therapy, folk remedies prepared at home can be used.
Purulent cervicitis
The causes of the formation of purulent cervicitis can be the presence in the body of gonococci, trachoma rods, ureaplasma. Signs of the onset of the disease are mucous secretions with impurities of pus and a specific smell. Edema forms inside the uterus, if you touch it with a swab during ectopia, blood is released. During the treatment of this disease, doctors give a recommendation to refrain from sexual intercourse.

Cervicitis during pregnancy
Inflammation of the uterus during gestation can lead to serious problems for the mother and baby. In the early stages, cervicitis during pregnancy provokes fetal fading, miscarriage. Then it will take a long time to be treated to get pregnant again. If the infection develops along the ascending path, the bacteria enter the uterus, causing placental insufficiency and abnormal embryo formation. Cervicitis in the later stages provokes delayed development in the child in the womb, infectious diseases, organ pathologies.
Cervicitis - causes
There are several factors that can cause cervicitis - the causes are classified as follows:
- Diseases that are transmitted through sexual intercourse: chlamydia, vaginosis, gonorrhea, candidiasis.
- Hormonal imbalances.
- Improper use of personal hygiene products, contraceptives.
- The occurrence in the uterine cervix of pathogenic microorganisms: staphylococci, fungi.
- Injuries of the mucous membrane during childbirth, etc.
Cervicitis - symptoms
The disease has the following characteristic features:
- During sexual intercourse or between menstrual cycles, spotting may occur.
- Sexual desire disappears, sexual intercourse provokes pain.
- Allocations with cervicitis have a pathogenic appearance: cheesy, foamy, purulent.
- There are false and frequent urge to urinate.
- A pulling pain appears in the lower abdomen.

Treatment of cervicitis
Having understood gynecology, explaining cervicitis - what it is, determining their type using a cytogram, you need to immediately begin treatment. Therapy should be carried out under the close supervision of a physician. Focal manifestations of the disease should be treated surgically. Treatment of chronic cervicitis is a complex of measures. Among the medications doctors prescribe:
- Candles for local use: Hexicon, Terzhinan.
- Group of antibiotics: Clarithromycin, Lomefloxacin.
- Means that restore microflora: Atsilakt, Bifidumbacterin.
- Correction of immunity: Immunal.
Physiotherapy is represented by the following methods:
- electrophoresis;
- exposure to ultraviolet rays;
- magnetotherapy;
- ultrasonic waves.
To maintain the body, additions to therapy, it is allowed to use folk remedies:
- Cotton swab moistened with garlic juice. Squeeze out the liquid from 2-3 cloves, mix with 1 tsp. apple cider vinegar and 1 tbsp. l. honey. Cotton wool should be moistened and placed inside the vagina, like a candle, for 60 minutes. The method cannot be used in the presence of erosion of the uterine mucosa.
- If cervicitis is provoked by candidiasis, take a steam bath by adding tea tree oil (a few drops). Carry out the procedure for at least 15 minutes.
With infectious cervicitis, drugs are prescribed:
- Ceftriaxone;
- Erythromycin;
- Flagyl;
- Livarol candles.
Video: chronic inflammation of the cervix
Attention! The information provided in the article is for informational purposes only. The materials of the article do not call for self-treatment. Only a qualified doctor can make a diagnosis and give recommendations for treatment, based on the individual characteristics of a particular patient.
Did you find an error in the text? Select it, press Ctrl + Enter and we'll fix it!Discuss
Cervicitis - what is this disease of the cervix. Symptoms and treatment of chronic and acute cervicitis in women
Cervicitis (from lat. cervix - neck) is inflammatory disease outer or inner part of the cervix. As a rule, it develops together with inflammation of the uterus and vagina, since all these structures are closely interconnected. The disease occurs in women of reproductive age and in the postmenopausal period. Often, cervicitis causes an infection that is sexually transmitted, especially if it is viruses,. An unpleasant feature of the disease is frequent chronicity and an imperceptible course, which leads to a belated diagnosis. Why is cervicitis dangerous and what consequences await a woman?
What is cervix?
The cervix or cervix is the narrowest part of the organ, a kind of entrance to the uterus. The uterus is a hollow muscular organ, which can be imagined as a bag, turned upside down. Its lower part looks like a dense tube several centimeters long - this is the neck. Inside it passes a narrow cervical canal, normally tightly closed and filled with mucus.
The cervix canal opens into the vagina - this is the vaginal portion or ectocervix. She is seen by a gynecologist when examining the patient's vagina. A woman herself can feel it with her fingers when inserting a hygienic tampon, vaginal suppository or cervical cap. The ectocervix looks like a pale pink disc with a hole or a small gap in the center.
During pregnancy, the cervix contracts tightly and holds the fetus with amniotic membranes and water in the uterus. Just before the birth, it softens and relaxes, and directly in the process of giving birth, the cervical canal expands up to 10 cm in order to let the baby out. Dysfunction of the cervix leads to miscarriage, violation of the biomechanism of childbirth.
The function of the cervix is a safe communication of the uterine cavity with the vagina. On the one hand, the cervical canal freely passes spermatozoa and menstrual blood, on the other hand, it reliably protects against the penetration of pathogenic microbes. It is filled with mucus, which is produced by the glands of the epithelium of the cervix. The consistency of mucus changes throughout the menstrual cycle. It is most fluid during the period of ovulation, in order to freely skip sperm and facilitate conception. Closer to menstruation and immediately after it, the mucus is dense, thick and contains a large amount of protective antibodies. Thus, it prevents the infection from being thrown from the vagina into the uterus and above.
The immediate causes of cervicitis in most cases are bacteria, viruses and protozoa:
- gonococci;
- trichomonas;
- genital herpes virus;
- human papilloma virus;
- streptococci;
- staphylococci;
- mycoplasmas;
- chlamydia;
- ureaplasma;
- mycobacterium tuberculosis;
- pathogenic fungus candida.
Of all these bacteria, only gonococcus is aggressive enough to penetrate the cervical mucus into the cervix and cause inflammation in it. Most other pathogens require additional factors to undermine the immune system and reduce protection:
- childbirth, abortion, miscarriage;
- surgery, endoscopic examination of the uterus, appendages;
- HIV infection;
- malformations of the reproductive system;
- chronic infectious and somatic diseases;
- hormonal imbalance;
- menopause;
- prolapse of the uterus and vagina;
- traumatic sexual intercourse;
- the use of irritating compounds for personal hygiene and contraception (one of the exotic methods is douching with lemon juice).
Immunity cells completely or partially eliminate the pathogen. In the first case, the disease completely disappears, and in the second it passes into a chronic stage. Some microorganisms are able to hide for years inside the cells of the epithelium and periodically cause an exacerbation of the disease.
The outcome of inflammation is the complete restoration of the cervix or excessive growth of connective tissue in it with the formation of adhesions. Prolonged cervicitis can lead to thickening of the cervical epithelium and blockage of the mouths of the mucous glands in its thickness. In this case, the secret accumulates inside the gland, gradually stretching it, which eventually forms a cyst. Such cervicitis is called cystic (follicular).
Types of pathology
Cervicitis is an extensive pathology, therefore, for convenience and understanding of the causes of the process, doctors divide it into different kinds. According to the duration of the flow, there are:
- acute - lasts no more than 6 months;
- chronic - lasts more than six months.
Depending on the cause, cervicitis can be:
- specific - it is caused by pathogenic bacteria (gonorrheal, viral, chlamydial, ureaplasma);
- nonspecific - develop under the influence of conditionally pathogenic microorganisms (staphylococcal, streptococcal, candidal). Often, an association of bacteria becomes the cause of inflammation - several of their species are isolated at once.
Nonspecific cervicitis is a consequence of a violation of the hormonal balance or the immune defense of the body. Specific, on the other hand, can develop against the background of complete health, if the pathogen is aggressive enough and enters the vagina in large quantities. Candidal cervicitis develops only against the background of severe immunodeficiency, for example, in women infected with HIV. Cervicitis is often observed during pregnancy.
In women during menopause, atrophic cervicitis develops, associated with a decrease in the concentration of estrogen in the blood. The secretory epithelium of the cervical canal produces an insufficient amount of mucus and becomes thinner, which leads to persistent sluggish inflammation.
The nature of the inflammation can be distinguished:
- purulent cervicitis - the cervical canal is filled with pus, the cause is usually gonococcus and opportunistic microflora;
- productive - healing processes predominate through excessive formation of connective tissue - scars, partitions;
- proliferative - chronic inflammation leads to the growth of the epithelium of the cervical canal with the formation of polyps.
Occasionally, cervicitis is allergic in nature. An inflammatory reaction can develop to latex, spermicidal agents, intimate lubricants.
How does the disease manifest itself?
The symptoms of cervicitis are so non-specific and blurred that often the patient does not pay attention to them and misses the acute stage of the disease. It may appear:
Signs of chronic cervicitis are quite difficult to track. It proceeds through the stages of complete calm and exacerbations, and inflammation during activation of the disease is expressed very moderately. The main symptoms of ill health that attract attention are vaginal discharge - cloudy, mucous, white or yellowish in color, practically odorless. There may also be pain during friction during sex.
Occasionally, a long delay in menstruation develops if the walls of the cervical canal are completely fused with each other. Chronic cervicitis is usually found during a screening examination, as it is not uncommon for a woman to have no signs of the disease.
How does inflammation affect pregnancy?
The cervical canal passes directly into the uterine cavity, as a result of which it is in close contact with the developing child, its membranes and waters. At a short gestational age, an ascending infection from the cervix can lead to damage to the embryo, its death and miscarriage.
At a later date, pregnant women also remain at risk of infection of the fetus, due to which it may lag behind in development or even die. In addition, there is a risk of developing cervical insufficiency. Thinned by years of inflammation, the cervix is not able to withstand the pressure of a growing child and opens ahead of time. This leads to premature birth and often to the loss of the baby.
Is it possible to get pregnant with cervicitis if the inflammation of the cervix lasts a long time? With intact patency of the cervical canal, there are no obstacles for the passage of spermatozoa and pregnancy can occur naturally. If the processes of formation of adhesions, scars predominate, or there is a complete fusion of the walls of the cervix, then the woman becomes infertile. Such infertility is considered reversible: restoration of cervical patency is performed surgically.

How is cervicitis diagnosed?
The diagnosis is established by a gynecologist based on the examination of the woman, the collection of anamnesis and familiarization with the symptoms of the disease. The fertile age of the patient, frequent change of sexual partners, neglect of condoms, and a recent sexually transmitted disease speak in favor of cervicitis. Moderate pain syndrome or its complete absence, unusual vaginal discharge also indicate inflammation of the cervix.
When examining on a chair, the doctor examines the vagina and cervix using a mirror. He sees inflammation of the vaginal portion of the cervix as an erosion of a bright red color on its surface. Unlike true erosion, the cause of which is a change in the type of epithelium on the cervix, cervicitis leads to the appearance of pseudo-erosion. It is inflammatory in nature, but the epithelium remains the same - flat multi-row.
Gonorrheal lesion manifests itself clearly: the cervix is swollen, bright red, pus oozes from the cervical canal. Trichomonas infection is characterized by a granular appearance of the ectocervix, outwardly it resembles a strawberry. Herpetic cervicitis occurs with severe inflammation: the cervix is red, a focal erosive process develops on its surface - an analogue of vesicles with fluid in herpes of a different localization. Bacterial cervicitis, caused by nonspecific microflora, also leads to the development of obvious inflammation with swelling and redness of the cervix.
Acute cervicitis leads to pain during the doctor's manipulations with the cervix, so taking a smear can be unpleasant and painful. A gynecologist with a special small brush scrapes epithelial cells from the cervical canal, the analysis of which provides rich information. The resulting material is used for microscopy - a cytogram of cervicitis is compiled. It is dominated by inflammatory cells (leukocytes), destroyed or modified epithelial cells.
The smear is also sown on nutrient media to grow bacterial or fungal colonies. Then they are examined to determine the microflora and its sensitivity to medicines. It takes at least 3-5 days before the results are obtained, therefore, with their help, the previously prescribed therapy is usually corrected.
With a persistent chronic course of cervicitis, a small piece of tissue is taken for analysis - a biopsy. The material is examined under a microscope and in special analyzers. A sign of chronic inflammation is lymphocytic cervicitis, in which the submucosal layer is filled with immune cells (lymphocytes).
Treatment of pathology
Treatment of cervicitis allows you to eliminate the cause of the disease, stop the inflammatory reaction, and restore the reproductive function of a woman. It is carried out on an outpatient basis, hospitalization and sick leave usually not required. If an STI pathogen is detected, both partners should be treated.
Treatment regimen for different types of cervicitis:
- for bacterial infections - treatment with antibiotics (candles Neomycin, Metronidazole), combined anti-inflammatory and antibacterial drugs (Terzhinan). After sanitation, suppositories with useful lactobacilli are prescribed to restore normal microflora (Acilact);
- with fungal infection - use antimycotics: inside Fluconazole, in the vagina - Natamycin tablets, suppositories with econazole;
- with chlamydial infection - a combination of several antibiotics (Tetracycline + Azithromycin) is prescribed for a period of at least 21 days;
- with atrophic inflammation, the introduction of suppositories, creams, gels containing estriol (Divigel) into the vagina helps.
Cysts, adhesions, adhesions, polyps of the cervical canal are surgically removed to restore the patency of the cervix.
Since cervicitis and erosion (pseudo-erosion) are essentially the same disease, after treatment, a woman needs to be seen by a gynecologist and go through. The inflammatory process on the cervix increases the risk of developing cancer, but a thorough examination using colposcopy allows you to identify it in its earliest stages and successfully eliminate it.
Cervicitis is a well-known problem in gynecology among women of childbearing age and is less common in the period before menopause. Establishing the real prevalence of the disease is somewhat difficult due to the fact that cervicitis is asymptomatic and is mainly detected during preventive medical examinations.
Cervicitis - what is it
The disease is a general inflammation of the uterus, which includes the presence of a pathological process in the mucous membrane of the vaginal part of the cervix and cervical canal. Separate inflammations are very rare, and in most cases are combined with other inflammatory problems of the female reproductive system (colpitis, vaginitis, cervical erosion).
ICD code 10 N72 Inflammatory diseases of the cervix.
Causes of Cervicitis
The mucous membrane of the cervical canal plays the role of a protective barrier between the uterine cavity and the external environment. The composition of cervical mucus includes proteolytic enzymes, immunoglobulins of all classes, bactericidal substances. As you can see in the photo, the cervix and its mucus are a kind of filter that provides protection from the influence of adverse agents.
The most common causes of Cervicitis can be:
- pathogens of sexually transmitted diseases: chlamydia, gonococci, trichomonads, papilloma and herpes simplex viruses, mycoplasma, ureaplasma;
- nonspecific flora: streptococcus, proteus, E. coli, Klebsiella, Candida fungi;
- trauma to the cervical canal during childbirth, abortion, the introduction of an intrauterine contraceptive;
- the action of strong chemical solutions when douching
- Changes in hormonal levels in premenopause can be the cause of Cervicitis.
It should be noted that an additional risk that contributes to the development of the disease is the early onset of sexual activity, the presence of sexual relations with a large number of men, childbirth before the age of 16, smoking, allergies to latex or spermicides, and taking certain hormonal drugs.
Disease classification
The disease is differentiated into several categories:
- according to the nature of the course of inflammation, there are acute, chronic and subacute cervicitis;
- by type of pathogen: specific and nonspecific Cervicitis;
- according to the degree of activity, minimal, pronounced and moderate cervicitis are distinguished.
Common symptoms of Cervicitis of the cervix
Inflammation is accompanied by the following symptoms:
- vaginal discharge of a foamy purulent nature, with an unpleasant odor;
- irritation and itching in the vulva;
- soreness during intercourse and sanious discharge after it, anorgasmia;
- pain in the lower abdomen and in the lower back of a pulling nature;
- burning sensation and pain during the act of urination;
- dark spotty vaginal discharge between periods.
If you notice these symptoms in yourself, contact your gynecologist immediately. Only on the basis of examination and diagnostic data, the doctor will make the correct diagnosis and prescribe the appropriate treatment.
In addition to the generally accepted classification forms of inflammation, there are other types of this disease.
Acute cervicitis: what is it
Inflammation that lasts up to 6 weeks. Symptoms are characterized by a rapid course, manifested by profuse purulent discharge from the vagina, moderately elevated temperature, pulling pains in the lower abdomen.
When examining the mirrors in case of acute inflammation, the gynecologist will see the release of pus from the external pharynx of the cervical canal, petechial hemorrhages, tissue swelling and redness of the mucosa, erosion may be detected.
Chronic cervicitis. APA.
Chronic cervicitis. Treatment, signs
Chronic cervicitis. Phonophoresis (NCUS)
In an acute form, gonococcal cervicitis occurs. The risk group for this disease includes women who have multiple sexual partners or a partner with gonorrheal urethritis. Purulent cervicitis is accompanied by copious purulent discharge and can spread into the uterine cavity.
Bacterial Cervicitis can provoke staphylococcus aureus, streptococcus and other nonspecific flora. The cause may be an imbalance in the vaginal flora, and the disease will not necessarily be associated with sexual activity.
Chronic Cervicitis
Chronic inflammation of the cervical canal mostly has no symptoms, and is detected when a woman contacts a doctor for other reasons. The chronic form of the disease can occur if the acute form of inflammation was not detected and treated in a timely manner. Due to the long-term pathological process, the formation of infiltrates, cysts and thickening of the cervix occurs, which makes it possible to determine the disease as productive Cervicitis.
Very often the cause of chronic forms are fungi, viruses or hormonal changes in the female body.
Candida cervicitis
Occurs in a situation where there is already a fungal infection in the vagina (thrush). When examining the cervix, white plaques are determined in the mirrors, which are easily scraped off, as a result of which the inflamed red mucosa is exposed.
Lymphocytic Cervicitis
The disease is also called follicular cervicitis. This form of inflammation is asymptomatic and occurs in menopausal women. The process is a lymphoid "impregnation" of the walls of the cervix, resulting in the formation of follicular benign formations. If this form of inflammation is detected, the doctor will definitely conduct a differential diagnosis with malignant lymphosarcoma.
Cystic cervicitis
It is a form of the disease in which the formation of benign cysts occurs in the cervical region. As a result of the inflammatory process, there is a blockage of the glands that secrete mucus and their subsequent growth, which the gynecologist will detect during examination or colposcopy.
Viral Cervicitis
The disease appears as a result of infection with the herpes simplex virus, human papillomavirus, HIV. Represents a certain difficulty in recognition, since it does not have specific features. During the examination, the doctor may see vesicles characteristic of a herpes infection, or only a laboratory will confirm the diagnosis.

Atrophic cervicitis
Most often it is a chronic and non-specific form of the disease. Frequent causes of atrophic inflammation are traumatic manipulations associated with a violation of the integrity of the cervical canal of the uterus or childbirth.
Diagnostics
To make the correct diagnosis, in addition to standard gynecological manipulations (examination in the mirrors, bimanual palpation), you will need to take a smear for a cytogram, sowing to determine the microflora of the vagina, donate blood to check for syphilis and HIV and major sexually transmitted infections. Diagnosis of the disease does not preclude colposcopy.
Why is Cervicid dangerous?
The main danger of the disease lies in its negative impact on the reproductive function of women. Patients who have suffered inflammation of the cervical canal in the future may have problems with conception and pregnancy, up to infertility. The long-term nature of the disease can also lead to oncological complications.
Treatment of cervical cervicitis
The main tactic in the treatment of the disease is the fight against the main cause, which served as inflammation. Given the clinic and laboratory data, the doctor will prescribe a comprehensive treatment.
Based on standards of care and feedback on the patient forums, you are presented with a list of drugs used for treatment.
Antibiotics for Cervicitis. Good feedback received the drug azithromycin, which has the name Sumamed, especially since its use is allowed in pregnant women. For the treatment of acute and purulent Cervicitis, fluoroquinolones (Ofloxacin), antibiotics of the tetracycline group are also used. Chlamydial Cervicitis is treated with azithromycin in combination with local treatment of the mucosa with solutions of Dimexide or Chlorophyllipt.
Candles for cervicitis: Hexicon, Terzhinan, Polygynax, Metronidazole.
Folk treatment of the disease
The essence of folk methods is to eliminate the consequences of the disease and strengthen the body's defenses. Decoctions of anti-inflammatory herbs are used: chamomile, oak bark, sage in the form of douches and tampons. Use folk remedies only after treatment prescribed by your doctor.
Watch your health!
The most interesting on the topic