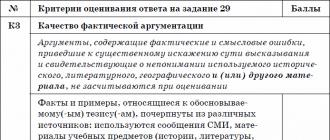
How does osteochondrosis manifest itself? Osteochondrosis: what kind of disease, symptoms, treatment, diagnosis, prevention. Treatment of osteochondrosis with drugs
Osteochondrosis is a pathology familiar to 40% of the population under the age of 35-40 years and almost 90% in old age. Even adolescents sometimes show signs of osteochondrosis - a decrease in the height of the discs, pain, discomfort in the spine. If you start treating the disease at the first stage, before the destruction of the disc, the chance to stop the progression is very high.
What is osteochondrosis?
With osteochondrosis of the spine, one or more intervertebral discs are damaged. The disease can occur in any department:
- chest;
- Shane;
- Lumbar (lumbosacral).
In severe cases, degeneration of the vertebral discs against the background of osteochondrosis is observed throughout the spinal column, which causes a person's disability. So what kind of disease is osteochondrosis? Pathology is associated with a gradual, steady and progressive malnutrition of the hyaline cartilages located on the intervertebral discs, as a result of which they change position, shape, and crack. A person experiences a strong pain syndrome, the functions of the entire musculoskeletal system are disturbed.
What is osteochondrosis regarding its consequences? If you do not carry out treatment, the vertebrae will shrink, the gaps between them will decrease, and the discs will begin to crush and collapse. This will lead to damage to the nerve roots, damage to the spinal cord and disruption of the internal organs. Bone osteophytes appear along the edges of the discs - growths that cause even more severe pain. The consequences of this disease of the spine are very serious.
Scientists have come to the conclusion, studying osteochondrosis, that this disease is a consequence of the upright posture of a person, so most people are prone to it. Daily high loads on the spinal discs, age-related deterioration of vascular function, malnutrition and aging of the body are the main causes of osteochondrosis. The following factors exacerbate the situation:

Injuries, heavy physical activity greatly aggravate the development of osteochondrosis of the spine. Therefore, in athletes, manual laborers, osteochondrosis of the lower back is a very “popular” problem. Heredity also plays an important role in the pathogenesis of the syndrome - if parents had serious back problems at a young age, the child has a high risk of getting a spinal disease.
Psychosomatic causes of pathology - a new direction in the search for prerequisites for its formation. Psychosomatics implies the influence of psychological factors on the development and course of physical illness. The connection between bodily and mental problems is really close, and a seemingly healthy person can suffer from regular pain. With osteochondrosis, some people do not find objective reasons for the pathology, but it continues to progress.
Up to 30% of patients after a visit to the doctor indicate such troubles as:
- Constant stress;
- Chronic experiences;
- Nervous tension;
- Family problems;
- conflicts;
- Moral breakdown.
In this case, the psychosomatics in the appearance of the spinal lesion syndrome is clearly traced - the person "bends" under the weight of problems, from which the spine suffers. If the pathology has similar causes, the treatment of osteochondrosis will be difficult, drugs usually do not help. Exacerbations of pathology occur during a new wave of stress, and there are no physical reasons for them.

Especially often, psychosomatics is reflected in the cervical spine, but the pain syndrome can be wandering throughout the spinal column. Treatment of osteochondrosis should begin with the search and solution of psychological problems under the supervision of a psychotherapist.
The intervertebral disc consists of liquid and solid parts. The first is in the center, representing a core that gives elasticity. From above, the core is surrounded by a strong ring. It is from the liquid structure that all pathological changes in the disc begin, which later spread to its shell.
In medicine, there are four stages in the development of osteochondrosis. This refers to the conditional division of pathology according to the severity of disorders in the spine:
- The first stage of osteochondrosis. The amount of moisture in the disc drops, it dehydrates. Destruction has not yet occurred, but after severe dehydration of the nucleus, microcracks begin to appear on the fibrous ring. There are usually no symptoms at this stage of the disease.
- The second stage of osteochondrosis. The height of the disk begins to decrease, which means the gradual addition of symptoms and the progression of pathology. In the spine, the distance between its individual segments decreases, due to which the ligaments sag. At this stage, in a number of patients, the disease causes slippage of the vertebrae - spondylolisthesis. Pain, discomfort occur during exacerbations, aching pain may be present even in remission.
- Third stage. Osteochondrosis of the spine at this stage gives a strong pain syndrome, because complications begin to form. Most often these are protrusions, disc prolapses, less often - arthrosis (degeneration) of the vertebral joints, subluxations of the vertebrae. Pain is supplemented by limited mobility of the affected segment of the spine.
- The fourth stage of osteochondrosis. The spinal column begins to adapt to the new conditions of existence, trying to fix the vertebrae in order to protect them from final destruction. For this, osteophytes grow, as if “immuring” the vertebra. The pain can be sharp due to injury to the nerve endings.

The first signs of osteochondrosis usually begin at the initial stage, when there is no pain yet. In the neck, lower back, less often - in the thoracic region, a crunch can be heard when moving (it means a violation of the nutrition of the disk, its dehydration). Further, when overloading, working in an uncomfortable position, a person may notice stiffness of the muscles of the back or neck. They become "stone" on one or both sides, which is uncomfortable, causes burning, irritation.
Subsequently, the symptoms of osteochondrosis become more pronounced. At rest, a person may feel normal, but work, lifting weights, sleeping on an uncomfortable pillow can provoke such phenomena:
- Aching pains;
- aches;
- Numbness of the hands (if the neck is affected);
- Feeling of stiffness;
- Forced decrease in movements;
- Muscle spasm;
- Shooting;
- Increasing pressure;
- Posture disorder.

When the patient's spine is overloaded, osteochondrosis gives more pronounced signs and symptoms. Pain occurs in the shoulders, gives to the arms, elbows, headaches appear. With osteochondrosis of the cervical region, there are tinnitus, dizziness, vertebral artery syndrome develops, vision is impaired. Over time, without treatment of osteochondrosis, muscle atrophy occurs, the skin becomes pale. The course of cardiac pathologies may be aggravated, the functioning of the liver, gallbladder, and gastrointestinal tract is disrupted.
The consequences of this disease are always unpleasant, they provoke an increase in pain. With osteochondrosis, there are:
- disc protrusion;
- Prolapse and herniation of the disc;
- Attacks of sciatica, sciatica, lumbago;
- Kyphosis, scoliosis.
The danger to a person largely depends on the type of hernia in osteochondrosis of the spine. They are anterior, posterior, lateral, and the most dangerous are posterior hernias - they can compress the spinal cord. In the lumbar segment of the spine, hernias are most common, mainly between 4-5 vertebrae.
Lumbar osteochondrosis can cause very unpleasant symptoms - backache (lumbago). The pain in lumbago is burning, sharp, unbearable, it is very difficult to endure. The cause is a pinched nerve, because the patient's neurovascular bundle is damaged. Especially dangerous in osteochondrosis is the cauda equina syndrome, when a large bundle of spinal nerves is pinched in a person. As a result, the functions of the intestines, the bladder suffer, and paralysis of the legs may even occur. 
Signs of osteochondrosis often come down to severe muscle atrophy. If the muscles do not participate in the work of the body for a long time, the movements of the spine are constrained, then individual fibers weaken. As a result, the patient may become an invalid, bedridden. Cervical osteochondrosis is also very dangerous, because a hernia in this segment can cause a violation of the blood supply to the brain. At this stage, there is a risk of impaired vision, swallowing, speech and other brain functions.
Having independently recognized the signs of osteochondrosis, you need to think about its treatment. Since the damage to the spine can reach different stages, the treatment of osteochondrosis will also be different. It is important to make the correct diagnosis so that the therapy is chosen correctly.
Due to the prevalence of the disease and the presence characteristic symptoms The doctor will be able to suggest a diagnosis already at a preliminary examination. But to differentiate osteochondrosis from other diseases of the back and internal organs, the following diagnostics are performed:
- Radiography of the spine. It will help to identify the height of the discs, the degree of their thinning, as well as the presence of osteophytes.
- CT, MRI. More preferred in the survey. With this disease, it will be possible to determine the severity of damage to nerves, soft tissues, to find the smallest protrusions.
With osteochondrosis, laboratory tests do not play a primary role, but the delivery of a general analysis, biochemistry is required to exclude inflammatory process, rheumatoid lesions of bones, joints. To study the function of the muscles, the doctor conducts a series of physical tests, and to clarify the work of blood vessels and nerves, they do duplex, electromyography.

If the symptoms and treatment of osteochondrosis are identified, it is not worth delaying therapy - the disease progresses rapidly. On the early stage gymnastics, massage to strengthen muscles are usually recommended - this will be enough. At other stages of osteochondrosis, medication will be needed, and sometimes surgery.
To relieve pain - the most unpleasant symptom of the disease - you can use non-steroidal anti-inflammatory drugs. They cannot cure osteochondrosis, but they are always prescribed before exercise therapy to relieve symptoms. In severe cases, drugs are administered in injections, but more often they are recommended in a course of 7-14 days in tablets and topically, in the form of ointments. The most popular NSAIDs for osteochondrosis are:
- Meloxicam;
- Ketorolac;
- Ketoprofen;
- Arcoxia;
- Dexalgin;
- Diclofenac.
If a person has a strong painful syndrome in the spinal area, he is given injections of glucocorticosteroids directly into the affected area. The drugs of choice are Diprospan, Kenalog. Short-term pain relief is possible with the help of blockades with Novocaine and other anesthetics.

Treatment of osteochondrosis is also carried out using the following means:
- B vitamins (Milgamma, Neuromultivit). Helps improve nerve conduction in the spine.
- Chondroprotectors (Artra, Dona, Alflutop). Nourish intervertebral cartilage, strengthen discs.
- Muscle relaxants (Mydocalm, Sirdalud). Reduce the strength of muscle spasms in osteochondrosis.
- Vascular preparations (Trental, Actovegin). Optimize blood circulation in the spine.
If osteochondrosis has developed, then only chondroprotectors are given for pain relief and pathogenetic treatment, they are taken in courses of 3-6 months. The rest of the drugs have a symptomatic effect and do not affect the course of osteochondrosis itself.
In the list of measures to treat osteochondrosis, physiotherapy methods are sure to appear. Thanks to physiotherapy, the treatment of osteochondrosis will be more effective, because the action extends directly to the focus of inflammation. Physiotherapy will relieve the painful syndrome, eliminate spasms, improve blood microcirculation, and help remove clamps from the nerves. The most popular methods are:
- Electrophoresis. Treatment of osteochondrosis in this way will allow you to deliver relaxing, anti-inflammatory substances and anesthetics directly to the zone of the vertebrae, muscles, ligaments.
- Ultrasound. It relieves unpleasant symptoms, anesthetizes, creates the effect of vibration massage, activates the metabolism at the local level.
- Magnetotherapy. Variable or constant magnetic fields anesthetize, eliminate the inflammatory process.
- Detensor therapy. In this disease, a person is placed on a special mattress with “ribs”, where the spine is stretched and massaged. At the same time, muscle tone improves.
All types of physiotherapy should be carried out in courses of 10-15 procedures, while individual contraindications must be taken into account.

Exercise therapy in the treatment of osteochondrosis plays a dominant role. Without exercise therapy, it will not be possible to form a strong muscular corset, and the latter is urgently needed to maintain a sick spine. Also, gymnastics enhances blood circulation in the area of the vertebrae, improves metabolic processes and helps to quickly remove decay products.
How to cure osteochondrosis with the help of gymnastics? The complex is selected only individually, and only at 1-2 stages it can be carried out without the supervision of a doctor. In the later stages, extra, more forceful movements can cause the disc to move and make the problem worse. At stage 3, all exercises are done only in the prone position.
For the treatment of osteochondrosis, massage is a must. In the acute stage, it is not done - it will cause a thrill. But a properly performed massage in the chronic stage with osteochondrosis is indispensable. After a course of sessions, muscles relax, clamps are removed, nerves and blood vessels begin to function normally. Massage is carried out only in a gentle mode, without sudden movements. You cannot trust your spine to a non-professional! 
The disease is most easily amenable to complex therapy if it is treated using different approaches. It is very important to improve nutrition in case of osteochondrosis - it should include vitamins, minerals, more food with gelatin, jelly, broths (if they are not contraindicated). So the nutrition of the cartilage will be improved, the discs will begin to recover.
Methods for treating osteochondrosis of the spine can be as follows:
- Manual therapy. The specialist physically affects the vertebrae, "puts" them in place when displaced, after which the result should be fixed by exercise therapy.
- Extraction, or traction. An effective method of treating osteochondrosis, carried out only with an individually selected load, quickly removes an unpleasant syndrome.
- Acupuncture. In the treatment of osteochondrosis, this method promotes the activation of blood circulation in the vertebrae, which relieves pain and improves cartilage nutrition.
- Orthopedic therapy. It involves wearing bandages that relieve pain and correct posture, as well as sleeping on special pillows.
There is also folk treatment osteochondrosis. These are the application of ointments, drinking herbal preparations, rubbing and herbal poultices. In complex therapy, such methods can be used, but they will not cope as the only remedy for this disease.

How to treat osteochondrosis if the situation has reached the destruction of the disc? Only surgery will help, because otherwise the person remains disabled. There are not so many indications for intervention, with osteochondrosis it is:
- Intractable pain (2-3 months or more);
- Disorders of motor function;
- Progressive muscle atrophy;
- Disk destruction;
- Complications from the nerves, spinal cord.
For the treatment of osteochondrosis, microdiscectomy (microsurgical operation) is most often recommended. It is performed by an experienced neurosurgeon to eliminate radicular compression. Part of the disc is removed, and it stops pinching the nerve. The doctor also removes bone osteophytes, which at an advanced stage of the disease can be voluminous. The disc itself remains in place, and the incision is only 1-2 cm.
With osteochondrosis, a more serious operation is the complete removal of the disc and its replacement with a graft. The vertebrae are fixed with iron devices. Unfortunately, in this place the spine will become immobile, but the nerve roots will be released. You can also place elastic silicone discs between the vertebrae - then the spinal column will fully retain its functions, but this intervention for osteochondrosis is quite expensive. 
In order not to bring to surgery for osteochondrosis, it is important to carefully consider the preventive measures:
- Do not allow hypodynamia. This disease can progress with power loads, but swimming, skiing, exercising will only benefit and help strengthen muscles and overall health.
- Follow your posture. At work and at home, it is important to sit correctly, not to stoop, and from childhood.
- Sleep on comfortable pillows. There are preventive pillows, with already existing osteochondrosis, several other, therapeutic ones are used.
- Don't lift weights. If necessary, you should sit down, stand with the object, keeping your back straight.
- Do exercises regularly to strengthen your muscles. This is important for the muscles of the neck, back, abs, lower back.
- Wear comfortable shoes. High-quality shoes (if necessary, orthopedic) do not develop flat feet - a risk factor for damage to the vertebrae.

It is also important to eat well, do not smoke, enrich the diet with vitamins, consume more fluids - this will reduce the likelihood of pathology.
Osteochondrosis is a serious disease of the spine, leading to disability. There are three types of disease: thoracic, cervical, lumbar. Everyone has symptoms.
A degenerative disorder in the articular cartilage affects the space between the vertebrae. Osteochondrosis destroys cartilage tissue, causing thinning. Everything around is inflamed, including nerve fibers. The vertebrae are gradually displaced, the nerves are pinched. In each section of the spine leads to certain symptoms, consequences. Neurological manifestations of osteochondrosis are considered important, serious.
The main symptoms of osteochondrosis
The main symptoms that occur with the types of the disease:
- Pain in the focus of the disease, aggravated at rest.
- Weakness in the body, present on waking, during the day. Caused by oxygen starvation.
- Jumps in blood pressure. It is characteristic of cervical osteochondrosis, occurs in other types of the disease.
The disease has vague, generalized main symptoms, and therefore requires careful diagnosis. Consider the neurological side of the symptomatology.
Neurology in cervical osteochondrosis
Cervical osteochondrosis is a type of dystrophic disorder that affects the vertebrae of the neck. Due to the progressive disease, a serious displacement of the vertebrae occurs. Symptoms are pronounced. The disease is common. Adolescents and younger children are often affected.
Neurological manifestations of dystrophic disorders in the cervical spine:
- Cervicalgia is present at all stages of cervical osteochondrosis. Expressed by dull pain in the deep tissues of the neck. Patients complain of a feeling of "a stake in the neck". Discomfort is present throughout the day, worse at night.
- Inflammation of the anterior scalene muscle is expressed by pain in the side of the neck, which radiates to the corresponding arm. Aching in the fingers on waking. It is caused by inflammation of the nerve fibers, the roots of the C5-C7 vertebrae.
- Cranialgia is characteristic of a severe form of osteochondrosis of the neck. It is expressed by a burning pain syndrome in the crown, above the eyebrows. Often, even powerful painkillers are not able to calm down.
- Cochlevestibular sensations are expressed by pain in the ears, crackling. Manifestations of cervical osteochondrosis require an urgent visit to the doctor. Blame oxygen starvation.
Cervical osteochondrosis has manifestations of neuralgia that require medical supervision. There are many arteries in the neck. The disease reduces blood flow, causing disturbances, failures. The main symptoms of the disease on the part of neurology are listed.
The manifestations of the disease are not obvious, it concerns the initial stage. Most go to the doctor when the disease has a second, third stage.

Neurology in thoracic osteochondrosis
Neurological manifestations of thoracic osteochondrosis:
- Aching pain under the shoulder blade - dorsalgia. The person is leaning forward. There is a feeling of fatigue in the back, unbearable heaviness in the upper part.
- Plexuses near the collarbone, ribs swell. Causes a feeling of discomfort when turning the back. The swelling is palpable under the shoulder blade.
- In the region of the atrium, a person experiences pain. Often there are no pathologies of the heart, the point is the xiphoid process, which becomes inflamed due to a back disease. The symptom is considered bright, common. Neurologists are faced with complaints of patients for pain in the heart. The disease does not affect the functioning of the heart.
These are the main symptoms of the manifestation of thoracic osteochondrosis in terms of neurological changes in the body. Symptoms are expressed by severe discomfort, pain. Analgesics, painkillers, psychotropic drugs used in severe forms of the disease will relieve pain.
These symptoms illuminate the manifestation of the disease in the thoracic region.
Neurology in lumbar osteochondrosis
Manifestations of osteochondrosis of the spine are from the side of the general condition, neurology. Osteochondrosis is a neurological disease, treated by a neuropathologist. Manifestation of a degenerative disorder in the articular cartilage of the lumbar region from the side of neurology:
- Lumboischialgia is a shooting pain that radiates to the leg. It manifests itself after a long stay in an uncomfortable position. It has a chronic, subacute form. Chronic lumboischialgia is common. A common symptom of lumbar osteochondrosis in the second stage.
- Lumbago is expressed as a shooting pain in the lower back, worse at night. There are types of lumbago. Each type differs in the nature of the pain.
- Nerve root disorders. Lower back pain is associated with the nerve roots in the back, which become inflamed, causing discord in the motor activity of the body.
Lumbar osteochondrosis is a common type of osteochondrosis. Every third patient suffers from a dystrophic disorder in the articular cartilage. Sometimes it appears in women after childbirth. Associated with injuries in the lumbar region, the pelvis, which occurred during the bearing of the baby, during childbirth.
Exacerbation of the disease is possible with subsequent births. Treatment is carried out comprehensively, fully. Taking most medications while breastfeeding is contraindicated. The doctor should find a way out of the situation by drawing up a scheme based on suitable medicines. Often, physiotherapy, traditional medicine is taken as the basis. A full-fledged treatment without medicines will not work, but the weakening of the effect of the disease on the body of a young mother is guaranteed.
The course of osteochondrosis
Denoting how osteochondrosis manifests itself, we note the stages of the course of the disease, characteristic of the varieties of the disease.
The acute course of the disease lasts 4 weeks. The patient feels a slight soreness in the inflamed area.
Subacute disease lasts up to three months. This is followed by a chronic course, lasting more than one year. Untimely, incomplete treatment threatens with serious problems in motor activity. Osteochondrosis can lead to disability, treatment should be taken seriously.
Therapy for getting rid of osteochondrosis is compiled by the attending physician - a neuropathologist. Self-treatment is excluded - the probability of positive dynamics without competent self-treatment is small.
After the main therapy, the body will need time to recover. The doctor will prescribe a course of physiotherapy, the use of methods traditional medicine. Traditional medicine recipes will shorten the recovery period, if used wisely. There are many plants, natural ingredients that help the body to fix the result after treatment.
The article was written for general educational development. To establish an accurate diagnosis and prescribe treatment, ALWAYS consult a doctor
Despite the fact that already in the initial stage of osteochondrosis, dystrophic-degenerative changes begin to appear in the body, this process can be stopped.
An integrated approach that consists of therapeutic and preventive measures can give a positive result. At the initial stage of the disease, it is important to reconsider your lifestyle and strictly follow all the doctor's instructions.
Degrees and stages
With timely treatment of osteochondrosis, it is possible to suspend
dystrophic-degenerative changes.
According to medical statistics, about half of people suffer from osteochondrosis to one degree or another. Today, osteochondrosis is not considered a disease of the elderly.
The vertebrae and discs in young people are increasingly exposed to degenerative changes. The risk group for osteochondrosis includes everyone without exception. The cause of the disease is a sedentary lifestyle, a monotonous activity.
Osteochondrosis is a disease with a degenerative-dystrophic nature that covers cartilaginous articular tissue, bone tissue, intervertebral discs with ligaments. As the disease develops, there is a limitation of mobility, with signs of infringement of soft tissues, vascular walls, and nerves.
The symptomatology of the disease and its treatment depend on the stage and where the dystrophic changes are localized. The clinical picture also depends on how affected and damaged the vessels, nerve endings.
The course of osteochondrosis has four stages:
- In the initial stage, clinical manifestations are mild or absent. The patient complains of mild back pain, which increases when the person starts to move. On examination, the doctor determines the local muscle tension. At the initial stage, migraine attacks, instability of blood pressure, numbness in the fingers, a sensation of noise in the head may begin.
- By the second stage of the disease, degenerative processes already cover the discs, the intervertebral spaces are reduced, and the fibrous capsule gradually begins to collapse. The patient complains of pain during movement, a feeling of weakness, reduced performance.
- By the third stage of the disease, the discs are completely displaced, the vertebral ring is destroyed. As a result, intervertebral protrusions are formed in the form of hernias with deformation of the spinal column. The patient complains of motor and sensory disorders in the area affected by osteochondrosis.
- To severe, the fourth degree of the disease, the patient has acute, unbearable, excruciating pain. Movement is difficult or impossible, sensitivity is impaired. If the focus is in the cervical segment of the spine, brain disorders develop.
It is a mistake to think that the initial signs of osteochondrosis are a temporary phenomenon, and the disease will go away on its own. Even the first signs make it clear that a serious and irreversible process is starting that requires treatment.
Untreated osteochondrosis will lead to hernias, chronic radiculitis, persistent neuralgia, limb deformities, and eventually to disability.
Diagnostics

If you find the primary symptoms of osteochondrosis, you should immediately consult a doctor.
Diagnosis of osteochondrosis begins with the collection of anamnesis. The doctor listens to complaints, finds out when the first symptoms appeared.
After that, radiography is shown in two projections, according to which the doctor determines the displacement and pathological mobility of the vertebrae, the degree of narrowing of the intervertebral spaces, the presence of osteophytes and seals.
At the next stage, it is shown with the help of which the doctor determines how compressed the nerve endings are and what pathological processes have occurred in the dura mater.
Localization
For osteochondrosis of the cervical spine in the initial stages, headaches are characteristic, which are not relieved by taking analgesic drugs. At the initial stage of osteochondrosis, pain is localized in the back of the head, gradually moving towards the temples.
The main sign of the initial stage of osteochondrosis: the pain syndrome in its intensity begins to increase if a person is in one position for a long time (sitting or standing).
At the initial stage of osteochondrosis, a headache is often combined with discomfort, decreased sensitivity in the hands. The patient may complain of pain in the neck or throat, painful sensitivity of the skin of the head, toothache.
With osteochondrosis in the thoracic region, the development of a cardiac syndrome is noted at the initial stage. The initial stage of osteochondrosis gives irritation to the roots of the nerve endings of the pectoral muscles and the phrenic nerve leading to the pericardium.

On the left is the initial stage of thoracic osteochondrosis, on the right is the post-initial stage of osteochondrosis.
At the initial stage of thoracic osteochondrosis, the patient complains of paroxysmal pain in the region of the heart. They are aggravated by coughing, sneezing, turning the torso. At the initial stage of thoracic osteochondrosis, tachycardia and drops in blood pressure may occur.
Read more about how to relieve and how to treat back pain with osteochondrosis of the spine, read this.
At the initial stage, thoracic osteochondrosis passes with imitation of other pathologies: cholecystitis, renal or intestinal colic. The patient may complain of difficulty swallowing, a feeling of tightness in the throat, bouts of pain in the stomach.
At the initial stage of lumbar osteochondrosis, the patient complains of aching lower limbs. It intensifies after physical activity, changes in body position, prolonged standing.
At the initial stage of osteochondrosis in the lumbar segment, the horizontal position of the body gives relief to the sick person. Also, pain and discomfort disappear after a person has changed the position of the body.
The initial stage of lumbar osteochondrosis is also manifested by backache, impaired sensitivity, chilliness of the lower extremities. With the development of the disease, paresis, paralysis and dysfunction in the work of the genitourinary system occur.
In the initial stage of sacral osteochondrosis, the main signs are similar to those of the lumbar. Sacral osteochondrosis is determined by the following feature: if a person lies on his back and raises his legs up, the pain begins to intensify and radiates to the buttocks and thigh.
Useful video about when to start treating osteochondrosis
Treatment

So that the degenerative process does not develop further from the initial stage of osteochondrosis, timely, adequate and regular treatment is essential.
Therapy of the early stage of the disease is complex and lengthy. All medical measures are aimed at eliminating all the symptoms of the disease.
Since osteochondrosis is a disease with dystrophic changes, treatment should restore cartilage, connective tissue, and nearby vessels.
Therapy of the early stage of osteochondrosis involves the appointment of vasodilators. Shown that stimulate the regeneration of cartilage tissue.
Osteochondrosis at an early stage is usually manifested by pain, so anti-inflammatory nonsteroidal drugs are also prescribed.
Drug treatment for osteochondrosis

Physiotherapy for osteochondrosis
Medical science has proven that osteochondrosis is an irreversible process. But it can be stopped. So that the degenerative process does not develop further from the initial stage of osteochondrosis, timely, adequate and regular treatment is essential.
Update: October 2018
V modern world almost all people over the age of 25 have this disease. Cervical osteochondrosis is much more common than in other parts of the spine. The relevance of this topic can hardly be overestimated.
In this article, we will consider why this disease occurs, how it manifests itself, how to treat cervical osteochondrosis, what drugs are effective in treating it, what non-drug methods exist, and we will also find out the answers to the most FAQ patients with a similar diagnosis.
Osteochondrosis of the cervical spine is a degenerative-dystrophic lesion (progressive) of the intervertebral discs in the cervical spine. For this reason, changes occur both in the intervertebral discs themselves, and in the vertebrae and joints of the cervical region themselves.
Causes of osteochondrosis of the cervical spine
As a result of the action of the following factors, there is an increase in the load on cervical region spine, neck muscles try to compensate for the excess load, their spasm occurs, blood circulation in this area is disturbed, which causes degenerative changes. Due to a number of factors, changes occur in the intervertebral discs of the cervical region, their structure changes, their nutrition is disturbed, changes occur in the small joints between the vertebrae, bone growths of the vertebral bodies appear, due to the increased load on the altered intervertebral discs.
Click to enlarge - Exercise therapy for osteochondrosis of any part of the spine
Factors contributing to the development of osteochondrosis of the cervical spine:
- Poor posture and scoliosis
- Overweight
- Hypodynamia, sedentary work
- Previous spinal injuries
- Metabolic disease
- Great physical activity
- Stress and constant nervous tension
- Low fitness level
- hereditary predisposition
- Habitual incorrect body postures, such as holding the handset with the shoulder
- Constant tension of the back, neck due to the peculiarities of work (stress in a sitting position) among drivers, office workers.
- Anomalies of development in the cervical spine
Degrees of development of cervical osteochondrosis
The degree of osteochondrosis is determined by the clinical picture and the patient's complaints. The concept of degree should not be confused with the stages of osteochondrosis. The stages will be discussed below.
First degree
clinical manifestations are minimal, the patient may complain of pain in the cervical spine of low intensity, it may increase when turning the head. Physical examination may reveal slight tension in the neck muscles.
Second degree
the patient is concerned about pain in the cervical spine, its intensity is much greater, the pain can be irradiated to the shoulder, to the arm. This occurs due to a decrease in the height of the intervertebral disc and infringement of the nerve roots. Pain is aggravated by tilting and turning the head. The patient may notice a decrease in efficiency, weakness, headache.
Third degree
symptoms of cervical osteochondrosis intensify, the pain becomes constant with irradiation to the arm or shoulder. There is numbness or weakness in the muscles of the arm, as herniated discs form (see). Worried about weakness, dizziness. On examination, there is a limitation of mobility in the cervical spine, pain on palpation of the cervical spine.
fourth degree
there is a complete destruction of the intervertebral disc and its replacement with connective tissue. Dizziness intensifies, tinnitus appears, and coordination is impaired, since the vertebral artery that feeds the cerebellum and the occipital lobe of the brain is involved in the process.
Clinical picture of osteochondrosis of the cervical spine - symptoms, signs
Symptoms of osteochondrosis of the cervical spine differ from the manifestations of this disease in other parts of the spinal column. This is due to the fact that in the cervical region the vertebrae are located closer to each other, the intervertebral discs have a relatively small height, which leads to the appearance of a clinic even with the most minor pathological processes. Also in the cervical region, compression of the nerve roots and spinal cord occurs more often.
The most common signs of cervical osteochondrosis are symptoms:
- Pain syndrome
pains can have different localization, they can be in the neck, in the occipital region, in the shoulder or upper limb. Pain in the shoulder or arm appears when the nerve root that innervates the upper limb is involved in the process. Pain in the occipital part of the head is caused by a spasm of the neck muscles that attach to the occipital bone and circulatory disorders in this area.
- Weakness in the arms
occurs when the root is damaged, which contains motor nerves that innervate the muscles of the hand.
- Decreased sensation in the hand
occurs when the root is damaged, which contains sensory nerves that innervate the skin of the upper limb.
- Restriction of movements in the cervical spine and crunching during movements
occurs due to a decrease in the height of the intervertebral disc, the appearance of bone growths on the vertebral bodies and damage to small joints between the cervical vertebrae.
- Dizziness, incoordination, weakness
all these symptoms are due to the involvement in the process of the vertebral artery, which runs in its own canal, located in the transverse processes of the cervical vertebrae. As a result of the development of cervical osteochondrosis, the formation of fibrous tissue, displacement of the vertebrae, the blood flow in these arteries worsens, which leads to a deterioration in the blood supply to the occipital lobe of the brain and cerebellum.
- Numbness of the tongue, decreased hearing and vision
occur in severe cases with a strong deterioration in the blood supply to the occipital lobe of the brain, cerebellum and trunk.
Symptoms depending on the damaged vertebra
Separately, radicular syndromes can be distinguished, leading to certain sensory and motor disorders. They differ depending on which vertebra compresses the spinal root: 
- C1: leads to numbness and impaired sensation in the back of the head;
- C2: pain in the parietal region and the back of the head;
- C3: violation of speech, sensitivity of the tongue, pain and decreased sensitivity in the direction where the spinal nerve is infringed;
- C4: pain in the heart, left hypochondrium, in the shoulder, shoulder blade, respiratory disorders, decreased tone of the neck muscles;
- C5: pain in the shoulder in the outer region;
- C6: pain radiating from the forearm to the thumb, and also from the neck to the shoulder blade;
- C7: pain in the back of the shoulder, from the neck to the shoulder blade, radiates to the forearm up to 2-4 fingers;
- C8: Pain from neck to shoulder, from forearm to little finger.
Diagnosis of cervical osteochondrosis
Main diagnostic methods:
- X-ray of the cervical spine. It is an uninformative method, especially in the later stages of the disease.
- CT scan. It shows changes in the vertebrae better, but it is difficult to determine the size and presence of intervertebral hernias, as well as the presence of disc-medullary conflict (compression of the spinal cord by a hernia).
- Magnetic resonance imaging. The most informative method. Not only bone structures are clearly visible, but also intervertebral discs, hernias, their size, direction of their growth.
- If you suspect a violation of blood flow in the vertebral arteries, apply ultrasonic duplex scanning. This method allows you to accurately determine whether there is a decrease in blood flow velocity, whether there are obstacles to normal blood flow.
X-ray stages of cervical osteochondrosis.
- Stage 1 - minimal changes in the configuration of the vertebrae, smoothness of the cervical lordosis (bending).
- Stage 2 - instability between the vertebrae, possible displacement of one vertebra relative to another, torsion (rotation around the axis of the spinal column), a slight decrease in the height of the intervertebral disc.
- Stage 3 - a decrease in the height of the intervertebral disc by ¼ relative to the disc located above, changes in the intervertebral joints, posterior osteophytes (bone outgrowths), narrowing of the intervertebral foramina and narrowing of the spinal canal, in which the spinal cord with its membranes is located.
- Stage 4 - a significant decrease in the height of the intervertebral disc, significant changes in the intervertebral joints, huge posterior osteophytes, a significant narrowing of the intervertebral foramina and a significant narrowing of the spinal canal with the formation of myelopathy.
Principles of treatment of cervical osteochondrosis
The main methods of treating osteochondrosis of the cervical spine are drug treatment, physiotherapy, massage of the cervical-collar zone, and therapeutic exercises are especially effective for cervical osteochondrosis. The main groups of drugs used in this disease include:
| Group name | Action | Dosage forms |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | reduce pain, help relieve aseptic inflammation and swelling of the root of the damaged nerve. | voltaren, nise, movalis, ketonal, ketanov, nimesulide and others (see the full list in the article). |
| B vitamins | improve metabolic processes in the nervous tissue. | combilipen, unigamma, neurobion (see) |
| Drugs that improve the rheological properties of blood and blood flow | improve nutrition of damaged nerve roots and improve blood flow to the brain. | eufillin, trental. |
| Chondroprotectors | drugs that restore cartilage tissue, including in a damaged intervertebral disc. | (glucosamine and chondroitin) artra, teraflex, doppelhertz, toad stone, kondronova, structuvit, alflutop. |
| Muscle relaxants | drugs that relieve muscle spasm. | , sirdalud, tizalud, tizanidine, etc. |
Attention! These drugs are not a prescription, they are presented for information only.
Physiotherapy in the treatment of cervical osteochondrosis
Physiotherapy
Exercise therapy for cervical osteochondrosis should be carried out without acute exacerbation. The greatest effectiveness of this technique during the recovery period. During the implementation of the complex there should be no discomfort and pain!
| Exercise #1 | Lying on your stomach, rest your hands on the floor, raise your head and torso, your back should be straight. Stay in this position for 1-2 minutes. Slowly lower yourself to the floor. Repeat 2-3 times. |
| Exercise #2 | Lying on your stomach, stretch your arms along the body, turn your head to the left, try to touch the floor with your ear, then turn your head to the right. Repeat 6-7 times on each side. |
| Exercise #3 | In a sitting position, while inhaling, lean forward and try to touch your chest with your head, then exhaling, lean back and throw your head back. Repeat 10-15 times. |
| Exercise #4 | While sitting, put your palms on your forehead, apply pressure with your palms on your forehead, and with your forehead on your palms. Continue this exercise for 30 seconds. Repeat 2-3 times. |
| Exercise #5 | Slowly rotate your head first in one direction, then in the other direction. 10 rotations in each direction. Watch out for dizziness. When it appears, the exercise stops. |
The most frequent questions of patients with cervical osteochondrosis and answers to them
Can surgery be required for cervical osteochondrosis?
Indications for surgical intervention are the lack of effectiveness of conservative treatment for 6 months, accompanied by constant pain and signs of damage to the nerve roots, as well as myelopathy. In all other cases, the operation is not performed.
How long can NSAIDs be used?
Since most NSAIDs have side effects on the gastric mucosa, prolonged and frequent use of these drugs is not recommended. When taking this group of drugs, you must strictly follow the recommendations of the attending physician, the duration of admission can be individual, it depends on the stage of osteochondrosis, the patient's complaints and his concomitant diseases.
How effective is it to take chondroprotectors?
At the moment, there is no evidence of the effectiveness and ineffectiveness of these drugs. In such cases, doctors are of the opinion that the drug is inappropriate to use.
What is the best way to get vitamins - in the form of tablets or injections?
There is no difference in the level of assimilation of drugs with these two routes of administration. Given the pain of injection and the frequency of complications, it is recommended to take B vitamins in tablet form.
What measures should be taken without exacerbation?
It is best to do physiotherapy exercises at home, attend a massage of the cervical-collar zone 2 times a year and limit excessive stress on the cervical spine.
The most common diseases of the spine are chondrosis and osteochondrosis. These two states have much in common, but there are also features. Let's try to figure out how one disease differs from another.
What is chondrosis?
From the name itself (chondro - cartilage) it follows that we are talking about a cartilage disease. If we talk about the spine, then we mean changes in the intervertebral disc and joints. The structure of the disk is very complex. In the center is the nucleus pulposus, which has a gel-like structure. It is surrounded by a fibrous ring, consisting of collagen fibers, closely intertwined with each other. The disc is separated from the vertebral bodies by thin hyaline cartilage.
Cartilaginous formations provide sufficient flexibility of the spinal column and perform a shock-absorbing function. The main role in the nutrition of the cartilage is played by the hyaline plate, through which the necessary substances penetrate into the center of the disc. Blood comes from the bodies of the vertebrae. In violation of metabolic processes, hyaline cartilage and collagen fibers are replaced by fibrous tissue. There is calcification and ossification of the plate adjacent to the vertebrae. The height of the discs is noticeably reduced.
The vertebrae are also interconnected by means of joints: arcuate, providing a connection between the processes, and atlantoaxial, located between the first and second cervical vertebrae. There is cartilage tissue here, undergoing the same changes as the discs. As a result, the function of the spine is impaired.
What is osteochondrosis
Osteochondrosis is a disease in which both cartilage and bone structures (osteo - bone) suffer. The ligamentous apparatus undergoes a change. This is the next stage after chondrosis, which is observed if you do not change your lifestyle and are not treated.
Over time, the disease progresses: osteophytes appear - growths of the vertebral bodies, hypertrophic changes in the facet joints (spondyloarthrosis), and hook-shaped joints. Ligaments thicken and calcify. Protrusions and intervertebral hernias may appear.
Clinical manifestations
Chondrosis may not manifest itself clinically. In some cases, there is an unexpressed pain syndrome and stiffness of movements. Changes in the intervertebral discs are detected only radiographically: decrease in height, deformation, displacement. On examination, pay attention to the curvature of posture.
Osteochondrosis has characteristic symptoms.
- Pain syndrome. Depending on the affected segment, pain occurs in the neck, thoracic or lumbosacral region. They can be in the form of lumbago, aching, stabbing. Possible irradiation in the arm, leg, under the shoulder blade, in the region of the heart. The pain is aggravated by movement.
- Root Syndrome. In addition to pain, sensory disturbances appear in the corresponding limb: numbness, burning along the nerve.
- With pronounced changes in the cervical vertebrae, the vessels passing in the intervertebral canal, which provide blood supply to the brain, may suffer. If the vertebral arteries are clamped, then there are signs of cerebrovascular insufficiency: nausea, vomiting, headaches, noise in the ears. Loss of consciousness is possible with a sharp turn of the head. Vegetative disorders in the form of excessive sweating, dilation or narrowing of the pupil, omission of the eyelid are characteristic. The sensitivity of the corresponding half of the face is disturbed.
- When the spinal cord is compressed by a hernial protrusion, the function of the organs located below the lesion site is disrupted.
X-rays show changes in cartilage, vertebrae, and ligaments.
Medical tactics
When chondrosis is detected and the initial manifestations of osteochondrosis, the treatment is somewhat different.
Drug therapy in both cases includes non-steroidal anti-inflammatory drugs and chondroprotectors. Unlike chondrosis, osteochondrosis can additionally be prescribed:
- muscle relaxants that reduce muscle spasm;
- drugs to improve blood circulation;
- B vitamins;
- hormonal agents that can be used as intramuscular injections or for blockade;
- blockade with lidocaine or novocaine.
Non-drug treatment is indicated in both cases:
- physiotherapy;
- the exclusion of heavy physical labor and a sedentary lifestyle;
- complete nutrition;
- getting rid of bad habits.
Additional therapeutic measures:
- massage and manual therapy;
- physiotherapy - electrophoresis, UVI, amplipulse, DDT;
- balneotherapy and mud therapy;
- acupuncture.
In severe cases with osteochondrosis, if there are hernias or compression of the spinal cord, they resort to surgical intervention.
Diagnosis and treatment is carried out exclusively by a doctor. It is dangerous for health to use medicines and carry out other procedures without consulting a specialist!
Thus, there is a difference between these pathologies, and it is significant, which is manifested in the symptoms and treatment approach. And yet, they are links in the same chain. If you start treating chondrosis in time, then the progression of the disease can be stopped and the development of osteochondrosis, which inevitably appears with age in all people, can be delayed.
Dorsalgia: pain in the lumbosacral spine
Throughout their lives, more than 50% of the population, one way or another, faced with various kinds of pain in the back. Among the elderly, you rarely meet someone who does not complain of bouts of pain in the lumbar region. Pain syndrome in the lumbosacral spine in medicine is designated by the general concept - dorsalgia.
- Causes of dorsalgia
- Disease classification
- Features of the clinical picture of the disease in the lumbosacral spine
- Diagnosis of dorsalgia
- Therapeutic measures
- Disease Prevention Measures
Doctors do not have a common opinion about whether any pain sensations in the region of the spinal column can be combined under this term. At first, the disease manifests itself episodically and the person does not attach any importance to this, but over time, the pain intensifies and causes a lot of inconvenience. Short-term attacks are replaced by a chronic course. There is a danger of complications such as inflammation of the spinal roots, up to serious malfunctions of the spinal cord.
 It may seem strange to many, but one of the main reasons for the development of dorsalgia lies in the psycho-emotional state of a person. Constant domestic stress, unfavorable family atmosphere and problems at work - all this affects the health of the back. By and large, the spine does not distinguish between physical and moral impact. In both cases, involuntary flexion of the back, curvature of posture and deformation of the vertebral structures occur. Everything else is added to excessive sitting at a computer desk, a lack of useful physical activity, and as a result, dorsalgia.
It may seem strange to many, but one of the main reasons for the development of dorsalgia lies in the psycho-emotional state of a person. Constant domestic stress, unfavorable family atmosphere and problems at work - all this affects the health of the back. By and large, the spine does not distinguish between physical and moral impact. In both cases, involuntary flexion of the back, curvature of posture and deformation of the vertebral structures occur. Everything else is added to excessive sitting at a computer desk, a lack of useful physical activity, and as a result, dorsalgia.
Causes of dorsalgia
There are several reasons that create conditions for dorsalgia of different parts of the spine:

Dorsalgia often occurs due to destructive degenerative-dystrophic processes inside the lumbosacral spine. Some diseases of internal organs are also capable of provoking an ailment.
Dorsalgia, as a rule, occurs with other morphological changes in the spine.
The list of spinal diseases associated with dorsalgia:
- A group of degenerative diseases (intervertebral hernias, osteochondrosis, spondylosis).
- Deformation diseases (kyphosis, scoliosis).
- Post-traumatic complications (fracture, dislocation, rupture of ligaments).
- Rheumatoid diseases (Bekhterev's disease).
- Malignant formations (osteosarcomas, osteomas, osteoclastoblasts).
- Infectious and inflammatory processes (tuberculosis, osteomyelitis).
Disease classification
According to the location of the painful focus, four types of dorsalgia are distinguished:

According to the method of occurrence, three forms of dorsalgia are known:
- Vertebrogenic. Caused by diseases of the spine, the pain spreads through the very body of the spinal column and the tissues surrounding it. Existing subspecies of this dorsalgia: inflammatory, degenerative, traumatic, oncological.
- Non-vertebrogenic. It is not caused by spinal problems themselves, but rather by indirect factors such as metabolic disorders or stress. It can be myofascial and psychogenic. In the first case, the picture of the disease is formed under the influence of bruises or inflammation of the muscle fibers of the back. In the second - under the influence of psychosomatic causes.
Like many other known diseases, dorsalgia has two clinical forms - acute and chronic. The acute form takes a person by surprise with its suddenness. With awkward turns, sharp shooting pains can occur. A fifth of all patients in 2-3 months are already faced with a chronic form of the disease.
Features of the clinical picture of the disease in the lumbosacral spine
Many people hold the view that minor pain is not a reason to rush to see a doctor. Such careless attitude to one's health is fraught with consequences. The spectrum of symptoms of lumbar dorsalgia is very wide. It is not always possible to understand the true cause of discomfort. So an intervertebral hernia at an early stage worries a person with acute unbearable pain, which makes it necessary to take painkillers. But at the last stage, the pain is almost imperceptible, which indicates atrophy of the nerve root.
 The first signal of the onset of dorsalgia will be a sharp sudden backache in the lower back. There are episodes when severe pain makes a person freeze for a few seconds. Chronic manifestations of dorsalgia are not so pronounced and do not differ in the aggressiveness of pain syndromes. Soreness is periodic, subsiding for a certain period after exacerbation. Postponing treatment, the patient thereby reduces the time of remission and dooms himself to constant pain.
The first signal of the onset of dorsalgia will be a sharp sudden backache in the lower back. There are episodes when severe pain makes a person freeze for a few seconds. Chronic manifestations of dorsalgia are not so pronounced and do not differ in the aggressiveness of pain syndromes. Soreness is periodic, subsiding for a certain period after exacerbation. Postponing treatment, the patient thereby reduces the time of remission and dooms himself to constant pain.
In order to recognize the dorsalgia of the lumbosacral region in time, you should pay attention to the following symptoms:
- The pain is sharp, aching, burning or throbbing. Localized in the lumbosacral spine. It can be both point and wide coverage.
- Decreased sensitivity of the skin in the affected area.
- Change in posture
- Difficulty moving the legs
- Pain and weakness in the legs
- Fainting state
- Body temperature is above normal
- Lower back pain when sneezing and coughing
As a rule, the symptomatic series is formed on the basis of the nature of the disease that provokes dorsalgia. Clinical studies confirm the close relationship between osteochondrosis and lumbar dorsalgia. After thirty years, the cartilaginous tissue of the spine is prone to wear and tear and natural destruction. Osteochondrosis is almost always a harbinger of more insidious diseases. This is a hernia and spondylosis. They add to the general symptoms of dorsalgia neurological disorders - paresthesias and malfunctions of internal organs. Osteochondrosis is notable for dull pain, which can be constant or in the form of attacks.
 Herniated discs are a fairly common disease that occurs in the lumbosacral region of the spine. The core of the pulp enters the spinal canal through the damaged sheath of the intervertebral disc. The longer and more intense this penetration, the more pronounced the compression of the nerves. Small hernias often do not manifest themselves. Lumbar back pain can be felt when inflammation occurs due to pinching of the radicular nerves. At the same time, the ligaments and muscles of the lumbosacral region are involved in the pathological process.
Herniated discs are a fairly common disease that occurs in the lumbosacral region of the spine. The core of the pulp enters the spinal canal through the damaged sheath of the intervertebral disc. The longer and more intense this penetration, the more pronounced the compression of the nerves. Small hernias often do not manifest themselves. Lumbar back pain can be felt when inflammation occurs due to pinching of the radicular nerves. At the same time, the ligaments and muscles of the lumbosacral region are involved in the pathological process.
Diagnosis of dorsalgia
The primary diagnostic measures used by the neurologist include talking to the patient and examining him. At the reception, the patient describes in detail the existing complaints. During the interview, the doctor is interested in the chronology of existing diseases in order to identify the possible mechanism of the current disease, its causes. This procedure makes it easier for the doctor to assess the severity of the problem.
 On examination, the specialist reveals the presence of visible deformation changes in the spine. The patient is asked to do a few simple manipulations with his hands to assess the safety of active and passive movements in the damaged spine. Palpation of the diseased area allows you to diagnose muscle clamps in the back frame. Neurological diagnostics is designed to exclude the presence of receptor disorders of the skin and evaluate reflex reactions.
On examination, the specialist reveals the presence of visible deformation changes in the spine. The patient is asked to do a few simple manipulations with his hands to assess the safety of active and passive movements in the damaged spine. Palpation of the diseased area allows you to diagnose muscle clamps in the back frame. Neurological diagnostics is designed to exclude the presence of receptor disorders of the skin and evaluate reflex reactions.
To establish an accurate diagnosis, the patient is given a referral to modern diagnostic methods:

Therapeutic measures
Treatment of dorsalgia both in the lumbosacral spine and in other departments is based on conservative methods and only in rare cases resort to surgical intervention. In the acute period of the disease and exacerbation of the chronic form, the patient is shown bed rest. It is advisable to equip the bed with orthopedic bedding: a mattress and a pillow. The most comfortable conditions will speed up the recovery time.
The mandatory treatment program includes a complex of medications selected by the doctor:

After the relief of pain syndromes, the patient is recommended to attend physiotherapeutic procedures: UHF, magnetotherapy, laser therapy, electrophoresis, exercise therapy, massage, swimming.
Disease Prevention Measures
It is worth adhering to simple measures to warn yourself against such an unwanted disease as dorsalgia:
- Every morning after waking up, perform a set of simple gymnastic exercises.
- Walk a daily distance of 5 km.
- Engage in strengthening the muscular corset, paying special attention to the large muscles of the back
- Prioritize healthy food
- Rationally distribute periods of work and rest. During breaks, do short workouts.
- Watch your posture while walking and sitting.
- Don't lift weights
- Seek medical attention if you suspect back problems