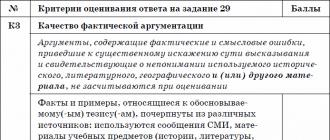
How to feed a child with exacerbation of gastritis. Can adults eat baby food with gastritis? What can cause gastritis
For the past few years, gastritis has been a confident leader among diagnosed diseases in both adults and children. True signs are bouts of severe abdominal pain, constipation, heartburn, nausea. In this situation, it is necessary not only to identify the disease and eliminate its causes, but also to pay special attention to baby food. From now on, it must comply with all strict rules and regulations. And don't forget to follow the instructions given by your doctor.
Symptoms and diagnosis of gastritis
Gastritis, like any other serious disease, goes through several stages: from acute to chronic. In any case, it is hazardous to health. Acute gastritis is a severe inflammation of the gastric mucosa. As a rule, the disease always begins suddenly: there is a sharp pain in the upper abdomen (just above the navel) or in the right hypochondrium, which is accompanied by nausea and even vomiting. Perhaps an increase in body temperature (up to 39 ° C), a disorder of the stool.
If your child has all of the above symptoms, then it's time to analyze what he might have eaten. After all, most often the acute form of gastritis is manifested by the use of any products (missing or harmful to health).
Today, there are several reasons why your child has gastritis. It could be:
- Food poisoning (check the expiration date of everything that the baby ate the day before);
- Eating foods that irritate the gastric mucosa;
- Reaction to medications and allergies.
At the first symptoms of acute gastritis, call your doctor immediately. In this case, it is impossible to do without diagnostics, which is carried out by experienced specialists. It is very easy for an incompetent person to make a mistake and not notice more serious surgical pathologies (appendicitis, intestinal obstruction, etc.).
Some diseases are life-threatening for a small patient, so it is the doctor who should help with the correct diagnosis. Call an ambulance, not a local pediatrician, because the first ones will arrive much faster. And do not refuse hospitalization: it is better to calmly leave the emergency room, knowing that there is no surgical pathology, than to worry and shudder for any reason.
Please note that after normalization of the condition, the child will want to eat. But the first three days, and that is how long the inflammation of acute gastritis lasts, nutrition should be limited to light dietary meals. For example, from cereals you can offer a child of oatmeal, rice, buckwheat. All of them should be cooked in water, not milk. Good for mashed potatoes. It should also be devoid of fat (i.e. no butter, gravy). In this case, vegetable broth soup is considered an excellent nutritious dish. By the way, do not buy fast food, as it can only worsen the condition of the child.
The diet for gastritis in children has its limitations. In no case should you give sausages, sausages, chips, crackers, chocolate, carbonated drinks. Give preference to steamed dishes, weak tea and compotes, dry biscuits and dried bread. It's great if you get a double boiler so that the food is nutritious and harmless. So, for example, you do not have to use sunflower oil and a lot of salt.
Thinking through the child's menu, consider the fact that meals should be fractional and frequent - 5-6 times a day. Serve warm, not hot or cold. Do not overfeed the child and try to strictly observe the regime these days: the little patient should sleep well, walk in the fresh air and eat only healthy food. With all the restrictions, diet food is extremely effective and often it is it that heals the body of babies.
If the acute process is overcome and treated fairly quickly, then the chronic form can last for years. Chronic gastritis is manifested by regular pain in the right hypochondrium, in the upper abdomen and umbilical region. At the same time, the child often feels sick, he is tormented by belching and heartburn, constipation and diarrhea, and often a lack of appetite is diagnosed. Also, a sure sign of not only chronic gastritis, but also other disorders of the gastrointestinal tract, are plaque on the tongue and bad breath.
However, the diagnosis of "chronic gastritis" in children is rarely made. There are several reasons for this. First, the doctor has the right to make such conclusions solely on the basis of certain studies, including after an endoscopic examination of the stomach (or gastroscopy). The procedure is unpleasant and not even all adults endure, let alone small children who are sensitive to any irritants. That is why they decide to take such a step only in the case when not one of the previously selected courses of treatment has not brought its positive results.
Important in the diagnosis is that abdominal pain, as a rule, is rarely associated exclusively with the stomach. World medical practice has long proved that in this case, children are diagnosed with functional disorders of several sections of the gastrointestinal tract at once: the liver and biliary tract, the intestines (primarily the intestinal microflora), and the esophagus. Incorrect work of the above organs has a bad effect on the condition of the stomach, which is indicated by frequent pains in this area.

Why did the child have gastritis
Naturally, chronic gastritis does not occur out of the blue. A number of factors contribute to this. Among them:
After you contact the clinic, the doctor will carefully examine the little patient, conduct tests and analyzes. Only after that, he will develop an individual treatment that will help in your particular case. In addition to medication, it includes a strict diet. After all, proper nutrition is always the basis of health, and in our case also a source of recovery.
Remember once and for all: the little man's menu is very different from ours. Dietary table number 1 is one of the fifteen tables that were developed by the Soviet nutritionist Mikhail Pevzner. Thanks to this diet, the inflammatory process decreases, ulcers heal better, and the secretory and motor functions of the stomach are normalized. Despite the restrictions that the diet contains, it is still balanced and contains the required amount of proteins, fats and carbohydrates.

Proper nutrition for gastritis
What not to eat during an exacerbation
First of all, you should clearly remember which foods should be excluded from the children's diet. So, the following are considered harmful:
- Any products made from rich and puff pastry (patties, buns), any fresh bread;
- Steep and fatty broths, strong vegetable broths (including stew), borsch on pork or lamb meat, okroshka and cabbage soup;
- Fatty meats and fish;
- Canned food and smoked meats, all kinds of sauces;
- Sour-milk products (kefir, curdled milk, fermented baked milk), salted cheeses, sour cream (allowed only in limited quantities);
- Fried and hard boiled eggs;
- Legumes, millet and corn porridge;
- White cabbage, sorrel, onion, cucumbers, home preservation;
- Acidic and fiber-rich fruits;
- Chocolate, ice cream;
- Carbonated drinks, strong tea and coffee.
What is the menu of the patient
Despite such a long list of prohibited products, you have a lot of useful things at your disposal:
- Dried bread, dry biscuits and biscuit;
- Boiled on water and pureed vegetables;
- Vegetable soups, milk porridges, puree soups;
- Meat boiled, steamed or baked;
- Low-fat fish, also steamed or boiled;
- Steam omelette or soft-boiled eggs (in this case, you must be sure of the quality of the egg);
- Milk, natural yogurt, non-acidic cottage cheese;
- Sweet berries and fruits (boiled and baked), jelly, jelly;
- Semolina, oatmeal, buckwheat, pasta, rice;
- As for drinks, it is best to give the child weak tea, juices, compotes, decoctions and water (purified from impurities and without gas).
When compiling the menu, do not forget that meals should be fractional and frequent, as indicated above. Make sure that your child does not eat dry food. Sandwiches cooked in haste can cause a serious aggravation. Ready-to-eat food should be at room temperature.
Never overfeed your children. Strictly observe the daily routine and be sure to walk with the baby at least two hours a day. Do not forget that, despite the disease, the child needs to develop. For this, amateur dancing or fitness classes are perfect. You can independently master with him a bicycle and roller skates in the summer, skates and skis in the winter. The main thing is not to neglect sports. After all, a sedentary lifestyle leads to a slowdown in metabolic processes in the body and poor absorption of food. And this is not the goal you are pursuing.
- 1st breakfast: steam omelet with vegetables, tea with milk.
- 2nd breakfast: baked apple with sugar.
- Lunch: pureed vegetable soup, steamed meatballs with boiled beets, fruit jelly.
- Afternoon snack: rosehip broth with crackers.
- Dinner: boiled or baked lean fish (no skin), mashed potatoes, a glass of juice or compote.
- At night: a glass of warm milk.
If your child has been diagnosed with gastritis (whether acute or chronic), don't panic and think that your loved one's healthy, fulfilling life is over. Perhaps it's just time to take a look at nutrition and physical activity in your family.
Diet can serve as an excellent basis for a daily diet. This is especially true if the child has chronic gastritis. Indeed, in this case, unfortunately, the body cannot be restored in a couple of days. And treatment can take years. But always look for the positives.
So, your child will form the concept of healthy and wholesome food, learn what is possible and what is not. Surely this will be useful in adult life. After all, to approach thoughtfully proper nutrition and not everyone can create a menu for themselves and their families. Arm yourself with patience, understanding and the desire to overcome the disease. After all, this is the only way to restore a young body and provide a child with a healthy and fulfilling life.
Talk 0
Similar content


The leading complaint of babies is pain in the abdomen. In most cases, discomfort causes gastritis in children. Symptoms and treatment should be discussed with the pediatrician. It is very dangerous to fight the disease on your own. Indeed, sometimes the disease is the initial stage of an ulcer. Only a doctor can conclude whether the damage to the gastric mucosa is superficial or massive.
Doctors, carefully examining gastritis in children, its symptoms and treatment, have selected many modern methods to cope with the disease. But only if the little patient will strictly comply with all prescribed appointments.
Causes of gastritis
Most people believe that the only culprit of the disease is malnutrition. However, the causes of gastritis in children are very diverse and lie not only in dry snacks. Consider those that in most cases lead to the development of the disease.

Types of gastritis
The disease is classified according to various criteria. Today, medicine distinguishes many varieties of such a disease as gastritis in children. The symptoms and treatment of each form differ accordingly. That is why it is quite important to consult a doctor if you suspect the development of an ailment.
In the course of the disease, gastritis is:
- Acute. Typical shape. It has pronounced symptoms. It provokes its occurrence with the wrong food, drugs, chemicals or mechanical damage. A bacterial source cannot be ruled out. As a rule, it always begins with the acute phase of the development of such an ailment as gastritis. Symptoms, treatment in children, ignored or misinterpreted, lead to the development of a chronic form. Such a transition can also provoke incorrect methods of dealing with the disease. An untreated disease also entails a more serious stage.
- Chronic. The form in which the course of the disease occurs almost asymptomatically. At the same time, chronic gastritis in children is characterized by morphological changes in the mucosa. Gradually, the regenerative ability of cells is lost. This leads to atrophy. The normal composition of hydrochloric acid, pepsins is disturbed. This immediately affects digestion.
- atrophic. Chronic gastritis in children, not treated for a long time, passes into the next stage. The atrophic form has no acute stages. It is, however, quite dangerous. The walls of the stomach become thinner and cease to regenerate. Soon the body may stop digesting food altogether.
According to acidity, gastritis is distinguished:
- with increased;
- with reduced;
- saved.
Symptoms of an acute form of gastritis
The signs that characterize the disease are very multifaceted. Among them are common, accompanying in children. However, there are specific signs that indicate the development of a particular form.
The acute stage is characterized by:
- Pain in the abdomen. It can be observed as paroxysmal, sharp form, and constant, dull. Feeling worse on an empty stomach.
- Heartburn, sometimes acid belching after eating.
- Nausea, often vomiting. The masses have a sour taste and smell. In some cases, the baby vomits bile.
- Dry mouth or increased salivation.
- Defecation disorder. May present as constipation or diarrhea.
- Weakness of the body, accompanied by dizziness and pain.
- Sweating, fever.
- Decreased blood pressure and increased heart rate.

General symptoms of the chronic form
As previously noted, a neglected disease acquires such a stage. Sometimes signs of development of this form are not very pronounced. Therefore, it is very important to carefully consider all manifestations.
In general, if the following is suspected in children:
- After eating (within 20 minutes) there is a slight dull pain.
- Lack of appetite, after eating, nausea occurs, a feeling of bloating or fullness appears.
- Belching accompanied by a putrid odor.
- Unpleasant taste in the mouth.
- Chair disorder. The child suffers from constipation and diarrhea.
- The surface of the tongue is covered with a gray coating.
- Anemia is diagnosed by a blood test.
- Hair becomes brittle, dry, nails begin to exfoliate.
- There is a general weakness. Often it is accompanied by increased drowsiness. Unreasonable irritability appears.
- Possible weight loss.
Treatment of gastritis

If the disease is caused by the bacterium Helicobacter pylori, then they begin with the elimination of the infection from the body. Before treating gastritis in children, the doctor will prescribe tests and recommend an examination. This will make it possible to establish the type, form of the disease. Therefore, to choose a set of effective measures to combat the disease.
When wondering how to treat gastritis in children, it should be understood that the basis of all methods is dietary nutrition. However, depending on the species, the acidity of the diet will vary.
For the stage of exacerbation is required. In some cases, this method manages to overcome all the accompanying gastritis symptoms. Treatment in children occurs even without the connection of medications. The dietary table simply makes it possible to "rest" the stomach and restore the mucous walls.
Physiotherapy is often connected to the correct one, special mineral waters are prescribed. If necessary, treatment is supplemented with enzyme preparations, antispasmodics. Their action is aimed at correcting vegetative disorders. Sedative therapy may be used.
Diet principles
Children should be based on the observance of certain rules.
- Regime diet. The child should eat 5 times a day. At the same time, it is important that the baby receives food strictly according to the schedule.
- Products and processing methods. All food offered to the child must be freshly prepared. All artificial additives, refined foods, sugar should be excluded from the diet. The most preferred processing methods are stewing, steaming and baking in the oven (without crust).
- Healthy foods. If acute gastritis is diagnosed in children, symptoms and treatment require a sparing diet. Preference is given to "mucilaginous" porridges. This is rice, barley, buckwheat. Semolina, oatmeal are also suitable. In the acute stage, raw vegetables and fruits are excluded. For any form of the course of the disease, it is forbidden to include canned food, fried foods, coffee, sweet teas in the diet. The following products are excluded from the child's menu: radish, white cabbage, spinach, radish, legumes.

Features of the diet in acute form
At this stage, the baby may experience dehydration as a result of vomiting. Therefore, it is very important to solder the child. The first 6-12 hours a small patient should receive only water and tea drinks. No juice!
Further nutrition for gastritis in children involves the inclusion of various soups ("mucous"). They must be ground with a blender. In the presence of heartburn, potatoes should be excluded.
After 3-4 days, the diet can be varied with steamed meat dishes - cutlets, meatballs. It is allowed to enter boiled fish in the menu.
On the 4-5th day, dairy food is connected. The child is allowed fruit juices.
Approximate diet
After recovery, the child is assigned table number 1. Below is an approximate diet for gastritis in children.
- Breakfast. Weak tea, you can with milk. Steamed omelette with a slice of yesterday's bread (white).
- Lunch. Rice (oatmeal) milk porridge. It is allowed to add butter - 0.5 teaspoon. A glass of cocoa or milk.
- Dinner. "Slimy" soup with vegetables. An egg is added if desired. Cutlets (meatballs) are exclusively steam. Small pasta. The food is washed down with weak tea.
- afternoon tea. Curd with fruit.
- Dinner. Chopped vegetables, rubbed through a sieve. Boiled chicken with a slice of yesterday's bread.

Diet for chronic gastritis with low acidity
The diet is signed by the doctor, usually for a week. If children with then the following diet is recommended.
- Breakfast. Buckwheat porridge, tea (not strong) with milk.
- Lunch. Boiled (stewed) vegetables. Rice cutlets with fruits. Cocoa.
- Dinner. Cereal soup on a "slimy" broth. Stewed meat with vegetables. Kissel.
- afternoon tea. Unsweetened cookies with a glass of yogurt.
- Dinner. Pancakes with cottage cheese or meat. Kissel (tea).

Approximate diet for high acidity
It should be understood that the diet for gastritis in children is compiled by the attending physician based on the diagnosis. Below is an approximate diet for reference.
- Breakfast. "Slimy" porridge. Tea.
- Lunch. Soft boiled egg. Fritters vegetable or steam cutlets.
- Dinner. Soup "slimy". Veal boiled with vegetables. Kissel or compote.
- afternoon tea. Sandwich with jam (cheese). A glass of milk.
- Dinner. Vareniki (pancakes) stuffed. Tea.
Conclusion
It is unpleasant, but not fatal, if gastritis is diagnosed in children. Symptoms and treatment require only an integrated approach. Besides medicines, the child needs strict adherence to dietary nutrition. This will save the baby from pain attacks and will contribute to a speedy recovery.
In recent years, there has been an alarming trend - many diseases of the gastrointestinal tract, previously observed only in adults, are significantly "younger". And more and more often, the diagnosis of "gastritis" is made to preschool patients 4-6 years old, which shocks parents. Even if you did not expect to face such a problem, at least remember that a positive result of treatment completely depends not only on drug therapy, but also on a properly selected menu.
How to feed a child with gastritis, so that it is tasty and healthy.Basic principles of nutrition for gastritis
In the treatment of such patients, particular importance is attached to the dietary table, its characteristics and accuracy of compliance. It depends on him how quickly the child will recover. In addition, properly selected nutrition has a beneficial effect on the work of the gastrointestinal tract between relapses of gastritis in children, increasing the interval between exacerbations in the chronic course of the disease.
- You need to eat fractionally. This is necessary in order to establish the secretory activity of the stomach, so regular meals 5-6 times a day instead of two or three plentiful feasts is the golden rule of any gastroenterologist patient, especially a minor.
- Products must be of good quality and fresh. It is unlikely that anyone would think of treating a sick child with smoked meats, but, nevertheless, do not forget that fatty, fried foods cooked in a large amount of oil or not properly heat-treated are categorically excluded.
- Food should not irritate the stomach lining. For this purpose, it must be brought to a homogeneous consistency by steaming or in water. In no case should the product be hot or cold, its optimal temperature should correspond to the temperature of the child's body, that is, be pleasantly warm.
- Balanced table. Banning certain foods doesn't mean you have to give up tasty food. On the contrary, a diet for gastritis in children from 4 years old involves a large assortment of first and second courses, snacks and sweets, and the child will receive everything necessary for healthy growth and development.

The more acute the condition, the more strictly these recommendations should be followed. Then, as the painful syndrome decreases and, you can gradually expand the baby's diet.
What not to feed a child with problems with the gastrointestinal tract
All foods that stimulate the production of gastric juice are highly discouraged for such a patient. The prohibited list definitely includes:
- fatty broths with fat;
- fried, salted, marinated dishes;
- any spices and sauces;
- “Heavy” food for the stomach, containing coarse fiber (the longer the product is digested in the walls, the more hydrochloric acid will be released). Do not give a child with gastritis products made from flour containing bran, winter apple peel, radish, cabbage;
- rich fresh buns;
- dried fruits - prunes, raisins, which are also removed from the stomach for a long time and cause fermentation processes in it;
- poultry liver, beef or pork. It filters and recycles everything that animals eat, being also a kind of cholesterol blow to the health of the child;
- carbonated drinks;
- canned food;
- nuts.
Unfortunately, the child will also have to give up chocolate, ice cream and most other store-bought sweets. These products always contain thickeners, dyes, additives that adversely affect the walls of the stomach and greatly slow down the healing process. What to feed a child with a sweet tooth: replace sweets with non-acidic fruits or berries in moderation.

What can be given to children with gastritis
Despite the seeming total ban on everything, the range of permitted food products is very rich. If your child was diagnosed with acute gastritis, then the baby food of the first days is the most careful attitude to the walls of the stomach and unloading the gastrointestinal tract.
When compiling the menu, be sure to consider the age and condition of the patient. There is a significant difference between the approach to treating an 8-year-old child and a very young child. If a student can organize sparing nutrition in the first days without harming the body, then for a three-year-old with an accelerated metabolism, even a few hours without food are unacceptable.
List of allowed dishes and products:

By preparing meals for every day from the above list of products, you will provide your child with a full range of essential trace elements and vitamins.
Nutrition for gastritis - an approximate menu for the day
It is important to observe the fragmentation of nutrition. Give your child as much food as he can handle, but don't let him feel hungry either. It is also important to maintain the correct balance of fluid in the body, with its constant companions - vomiting and diarrhea. Give your child plenty of water to prevent dehydration.
Thus, gastritis, contrary to popular belief, is not a "culinary sentence" at all. It is possible to feed a child tasty and varied even within the framework of the most strict diet. Healthy nutrition will be the key to the recovery of your child and, importantly, from an early age will gradually form in him the right ideas about the culture of food.
The key to a quick and effective recovery from gastritis is proper and healthy nutrition. Baby food, in turn, is enriched with vitamins, micro and macro elements, it does not contain preservatives and it is convenient to use. The list of benefits should reassure the patient suffering from gastritis that the use of foods for children will help them to properly treat the disease.
Diet for sickness
There are principles of nutrition. A patient who follows the rules of a healthy diet will ensure high efficiency of therapy. Diet rules for gastritis are as follows:
- The possibility of overeating should be excluded. Servings no more than 200 g.
- You need to take food in a fractional way. 5-7 per day in portions, small in volume.
- The consistency of food is soft, enveloping the walls of the stomach.
- Food temperature is not more than 36-38 degrees. Such food will not irritate the walls of the stomach.
Advantages and disadvantages
 Baby food has a completely natural composition.
Baby food has a completely natural composition. Baby food has a number of advantages over simple food. Among them are the following items:
- product quality (checked by sanitary and hygienic authorities);
- no food additives, flavor enhancers, GMOs, preservatives, dyes;
- ease of transportation;
- affordable variety of products (meat, vegetables, fruits).
Disadvantages of baby food for gastritis in adults:
- high cost of products;
- low calorie;
- small amount of fiber.
Baby food for adults with gastritis
With their characteristics, such products outperform simple dishes, but the question of whether they can be used for gastritis in adults is acute. It is impossible to answer negatively. Such food does not have enough fiber, dietary fiber, which perform a particularly important task in the process of forming the environment of the intestinal tract, but on the other hand, such products are very useful, all dangerous and unhealthy substances and a lack of vitamins and microelements necessary for the body have been extracted from them, can be offset with greens and whole grains. The conclusion is this: the diet for gastritis should not consist only of baby food. It needs to be enriched with foods full of fiber and dietary fiber.
Acidity
 After heat treatment, vegetables are less irritating to mucous membranes.
After heat treatment, vegetables are less irritating to mucous membranes. If such a diagnosis is made to an adult, then the menu should contain mucous cereals, fruits and vegetables. Products should not be consumed in their natural form. They should be baked or made into a stew. The following foods should be included in the diet for the treatment of the disease:
- lingering cookies, crackers or oven-dried bread;
- milk, dairy products;
- vegetable slimy soups;
- pasta;
- marmalade, marshmallow and marshmallows;
- boiled meat or in the form of mashed meat (chicken, turkey, rabbit, veal);
- fish products;
- jam and honey;
- steamed omelet (the number of eggs per week is three pieces);
- seafood;
- peas, greens and non-acidic berries;
- vegetable oil;
- kissels from non-acidic fruits, compotes, uzvar, tea.
Allowed foods for low acidity
 Diet will help eliminate the inflammatory process.
Diet will help eliminate the inflammatory process. It must be remembered that the goal of therapy is to reduce the inflammatory process. Then they cause additional production of their own gastric juice. The list of products for patients with low acidity is as follows:
- tea with low-fat cream and milk, lemon water with added sugar, berry and fruit non-acidic juices;
- crackers made from white wheat varieties;
- lingering cookies;
- a moderate dose of butter;
- low-fat cottage cheese bought at the store;
- soft-boiled eggs;
- steamed omelets;
- vegetable soups;
- cereals;
- boiled lean meat in the form of mashed potatoes;
- steam cutlets;
- pasta;
- lean fish;
- greens and vegetables (it is necessary to exclude sorrel and spinach);
- berries of sweet varieties;
- uzvar, compotes.
With the gradual treatment of the mucous membranes of the walls of the stomach, it is necessary to introduce food in small doses that stimulates the formation of gastric juice. Add more raw, fresh vegetables and fruits to your diet. Shredded food is replaced with food with fine cuts.
9230 0
Nutrition for acute gastritis (OG)
Acute gastritis (inflammation of the gastric mucosa) can occur in children due to gross eating disorders: consumption of poor-quality foods, intake of large amounts of fatty or rough, fiber-rich foods (immature fruits, berries), eating disorders, eating hastily or dry food.Acute gastritis is manifested by nausea, sometimes vomiting, belching, pain, a feeling of heaviness in the epigastric region.
The best medicine for OH is abstaining from food intake during the first day.
At the same time, the inflamed gastric mucosa rests, which is a kind of protective measure, since the release of digestive juices during inflammatory process decreases sharply.
It is only necessary to give the child often and in small portions during this period warm, weak tea, boiled water, weak decoctions of herbs without sugar, 5% glucose solution in combination with physiological saline (0.9% solution table salt). The total amount of fluid is determined by the degree of thirst in the patient.
The next day after fasting, fruit and vegetable and cereal decoctions, rosehip decoction are allowed. From the third day of illness, the child is transferred to liquid food: weak fat-free broth with white crackers or slimy pureed soup, jelly, liquid cereals.
Only from the fourth day meat steam dishes (meatballs, meatballs), boiled fish, various puddings are included in the diet. On the fifth day, you can already use milk soups, boiled chicken (without skin), thicker cereals and vegetable puree(potato, carrot). Then the child is gradually transferred to a normal diet in accordance with age, expanding the methods of culinary processing of products. Steam dishes are replaced with boiled ones, instead of jelly they give fresh fruit puree, fruit juices, baked apples.
To prevent chronic gastritis for several weeks, spicy and salty foods and indigestible fatty foods should be excluded from the diet of a child who has recovered from OH for several weeks.
Nutrition for chronic gastritis (XT)
Chronic gastritis occurs mainly in children of preschool and school age. With chronic hepatitis, the stomach glands that produce hydrochloric acid, pepsin and mucus are affected. As a result, the activity of the stomach is disrupted.Moreover, violations can be of two types: in one case, the level of hydrochloric acid increases (CH with increased secretory activity), in the other it decreases (CH with reduced secretory activity).
The main manifestation of chronic gastritis is pain in the epigastric region, most often after eating, accompanied by heartburn or acid belching with increased acidity of gastric juice, nausea, loss of appetite and belching with air - with low acidity.
It should be noted that in conditions of inflammation and atrophy of the gastric mucosa, its absorption capacity is enhanced. At the same time, large molecules of nutrients begin to be absorbed, which leads to intoxication and allergization of the body. In children, the general state of health worsens, they quickly get tired, food allergies appear or intensify.
With chronic hepatitis with normal or increased secretory function of the stomach, the child should eat 6-7 times a day in small portions, as a result of which free hydrochloric acid, which irritates the stomach, does not have time to form.
At the same time, foods and dishes that have a local irritant effect on the inflamed gastric mucosa, as well as having a strong juice effect are excluded from the diet of a sick child: meat, fish, strong vegetables, especially mushrooms, broths, cabbage broth, fried meat and fish, raw unmashed vegetables and fruits, pickles, marinades, smoked meats, spicy snacks, sausages, canned food, fresh onions, radishes, turnips, radishes, wheat porridge, black bread, pies, pastry pastries, cold and carbonated drinks, ice cream, sour berries and fruits .
Dishes are prepared from boiled products and given in a pureed form. Meat and fish are boiled in two waters and passed through a meat grinder, cereals and vegetables are rubbed.
Valuable products for the nutrition of such patients are milk (3-4 glasses of warm milk to reduce the acidity of the contents of the stomach), cottage cheese, eggs.
Fats should not be limited in their diet, but dishes containing simple carbohydrates (sugar, sweets) in the diet of such children should be somewhat reduced.
From raw vegetables, only grated carrots and finely chopped tomatoes seasoned with sour cream or vegetable oil, as well as raw, finely chopped greens, are allowed. The remaining vegetables should be boiled and salads should be prepared from them, but without adding onions.
The first courses are prepared in the form of vegetable puree soups (except cabbage) on cereal broth or milk soups with pureed cereals or noodles with vegetables. For the preparation of second courses, chicken, lean beef, fish, boiled in water or steamed, are used.
To improve the taste after boiling, they can be lightly baked in the oven. For the preparation of second courses, eggs, cottage cheese, sour cream, cream are used. As side dishes for meat and fish dishes, you can offer mashed potatoes and carrots, boiled cauliflower, beets, stewed or mashed zucchini and pumpkin, as well as boiled noodles, vermicelli, cereals. The latter are also given as an independent dish for breakfast or dinner. Dishes are seasoned with butter or vegetable oil, you can use sour cream and milk sauces.
For breakfast and dinner, in addition to the named dishes, it is recommended to steam various puddings, omelettes, casseroles, as well as milk porridges. Of the bread products, they use white wheat stale (yesterday's) bread, white crackers, unbread cookies, biscuit.
Food for children with chronic hepatitis with normal or increased secretion of the stomach, it is desirable to slightly undersalt, and spices should be excluded altogether.
Depending on the age of the child, it is recommended to include in the daily diet 650-800 ml of milk, 35-50 g of butter, 25 g of vegetable oil, 50-60 g of sugar, 110-120 g of fresh fruit, 140-210 g of potatoes, 90 -140 g of vegetables, 55-85 g of cereals (including pasta), 150-250 g of wheat bread (including all types of bakery products). Cottage cheese is given 3-4 times a week, 45-65 g per day, mild cheese is used on days when there are no curd dishes on the menu. Cheese is usually added grated to butter, preparing a sandwich for breakfast or dinner (weekly rate 45-55 g).
During the period of exacerbation of chronic hepatitis with normal or increased secretory function of the stomach in the first week, the child is given food 6-8 times a day, slightly reducing its total volume and set of products. The basis of the diet at the beginning of an exacerbation of chronic hepatitis is milk, the volume of which increases to 1 liter per day.
You can also use cream, soft-boiled eggs or in the form of steam omelet(1-1.5 pieces per day), butter (15-25 g per day), pureed cottage cheese (30-45 g per day), slimy pureed cereal soups, pureed milk porridges, steamed puddings, meat and fish soufflés and hashé from boiled products, white crackers, small amounts of fresh fruit (for making jelly). Less salt is added to food than for healthy ones.
Such a diet (see diet No. 16 below) is prescribed to a sick child for 1-2 weeks. But since it is close to physiological and almost completely satisfies the needs of the child's body for proteins, fats and carbohydrates, in the case of a slow recovery process (this is evidenced by ongoing pain, heartburn and other disorders), it can be extended for another week.
From the third or fourth week of treatment, the menu of a sick child is gradually expanded, the number of feedings is reduced to 5-6, and the calorie content of the daily diet is increased. In nutrition, gradually reduce the volume of milk and increase the content of butter, cottage cheese. Vegetable oil, stale wheat bread, boiled vegetables, fresh non-acid fruits, dried fruit compote are introduced into the diet. All food is given in pureed form.
Then, for 6-12 months, the child should eat the same foods and dishes, but cooked without rubbing and sharp mechanical grinding. Several times a week, you can eat well-baked lean buns, cheesecakes with cottage cheese, pies with apples, boiled meat or fish, eggs. It is not contraindicated to use milk sauce as a gravy (without sautéing flour) with the addition of butter, sour cream, as well as fruit and milk-fruit sauces.
Below are exemplary one-day menus for children with CG with normal or increased secretory function of the stomach during an exacerbation (diet No. 16; Table 20) and without an exacerbation (diet No. 1 pureed and No. 1 non-purified; Table 21).
Table 20. Approximate seven-day menu for a child with exacerbation of chronic gastritis with normal or increased secretion, or with peptic ulcer of the stomach or duodenum (diet No. 16)
|
Feeding |
Name of the dish |
Serving, g, ml |
||
|
3-6 years old |
7-10 years old |
11-14 years old |
||
|
After sleep 20-30 minutes before meals | ||||
|
First breakfast |
fish pudding Liquid potato puree | |||
|
Lunch |
Milk jelly | |||
|
20-30 minutes before lunch | ||||
|
Creamy oat milk soup Steam meat cutlets mashed rice porridge Kissel from dried fruits White bread crackers | ||||
|
Curd cream | ||||
|
Pureed buckwheat milk porridge Soft-boiled egg White bread crackers | ||||
|
Milk | ||||
Table 21. Approximate one-day menu for a child suffering from chronic gastritis with normal or increased secretion or peptic ulcer of the stomach or duodenum, in the stage of fading exacerbation (wipe diet No. 1) and in the period without exacerbation (wipe diet No. 1)
|
Feeding |
Diet number 1 pureed |
Diet number 1 unmashed |
Serving, g, ml |
||
|
3-6 years old |
7-10 years old |
11-14 years old |
|||
|
After sleep 20-30 minutes before meals |
Infusion of yarrow, chamomile and plantain |
Infusion of yarrow, chamomile and plantain | |||
|
First breakfast |
Natural steam omelet Carrot puree Surrogate coffee with milk White bread with butter |
Natural steam omelet Salad of boiled carrots with vegetable oil Surrogate coffee with milk White bread with butter | |||
|
Lunch |
Baked apple with sugar |
Baked apple with sugar | |||
|
20-30 minutes before lunch |
Cabbage or potato juice |
Cabbage or potato juice | |||
|
rice milk soup Steam meat cutlets Mashed potatoes Dried fruit compote, grated White bread |
rice milk soup Steam meat cutlets Mashed potatoes Dried fruit compote White bread | ||||
|
Cookies |
Cookies | ||||
|
Tea with milk White bread with butter and grated cheese |
Porridge from oatmeal"Hercules" dairy Tea with milk White bread with butter and cheese | ||||
|
Milk |
Milk | ||||
V.G. Liflyandsky, V.V. Zakrevsky